Hypoglycemia, also spelled hypoglycaemia or hypoglycæmia, sometimes called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose below 70 mg/dL (3.9 mmol/L), symptoms associated with hypoglycemia, and resolution of symptoms when blood sugar returns to normal. Hypoglycemia may result in headache, tiredness, clumsiness, trouble talking, confusion, fast heart rate, sweating, shakiness, nervousness, hunger, loss of consciousness, seizures, or death. Symptoms typically come on quickly.

An insulin pump is a medical device used for the administration of insulin in the treatment of diabetes mellitus, also known as continuous subcutaneous insulin therapy. The device configuration may vary depending on design. A traditional pump includes:
Intensive insulin therapy or flexible insulin therapy is a therapeutic regimen for diabetes mellitus treatment. This newer approach contrasts with conventional insulin therapy. Rather than minimize the number of insulin injections per day, the intensive approach favors flexible meal times with variable carbohydrate as well as flexible physical activities. The trade-off is the increase from 2 or 3 injections per day to 4 or more injections per day, which was considered "intensive" relative to the older approach. In North America in 2004, many endocrinologists prefer the term "flexible insulin therapy" (FIT) to "intensive therapy" and use it to refer to any method of replacing insulin that attempts to mimic the pattern of small continuous basal insulin secretion of a working pancreas combined with larger insulin secretions at mealtimes. The semantic distinction reflects changing treatment.
The following is a glossary of diabetes which explains terms connected with diabetes.

Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of diabetes mellitus. Signs and symptoms may include vomiting, abdominal pain, deep gasping breathing, increased urination, weakness, confusion and occasionally loss of consciousness. A person's breath may develop a specific "fruity" smell. The onset of symptoms is usually rapid. People without a previous diagnosis of diabetes may develop DKA as the first obvious symptom.

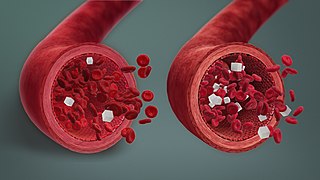
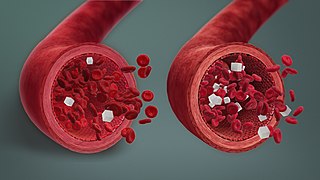
Hyperglycemia or hyperglycaemia is a condition in which an excessive amount of glucose (glucotoxicity) circulates in the blood plasma. This is generally a blood sugar level higher than 11.1 mmol/L (200 mg/dL), but symptoms may not start to become noticeable until even higher values such as 13.9–16.7 mmol/L (~250–300 mg/dL). A subject with a consistent fasting blood glucose range between ~5.6 and ~7 mmol/L is considered slightly hyperglycemic, and above 7 mmol/L is generally held to have diabetes. For diabetics, glucose levels that are considered to be too hyperglycemic can vary from person to person, mainly due to the person's renal threshold of glucose and overall glucose tolerance. On average, however, chronic levels above 10–12 mmol/L (180–216 mg/dL) can produce noticeable organ damage over time.

Type 2 diabetes (T2D), formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent urination, fatigue and unexplained weight loss. Other symptoms include increased hunger, having a sensation of pins and needles, and sores (wounds) that heal slowly. Symptoms often develop slowly. Long-term complications from high blood sugar include heart disease, stroke, diabetic retinopathy, which can result in blindness, kidney failure, and poor blood flow in the lower-limbs, which may lead to amputations. The sudden onset of hyperosmolar hyperglycemic state may occur; however, ketoacidosis is uncommon.

The blood sugar level, blood sugar concentration, blood glucose level, or glycemia is the measure of glucose concentrated in the blood. The body tightly regulates blood glucose levels as a part of metabolic homeostasis.

Gestational diabetes is a condition in which a woman without diabetes develops high blood sugar levels during pregnancy. Gestational diabetes generally results in few symptoms; however, it increases the risk of pre-eclampsia, depression, and of needing a Caesarean section. Babies born to individuals with poorly treated gestational diabetes are at increased risk of macrosomia, of having hypoglycemia after birth, and of jaundice. If untreated, diabetes can also result in stillbirth. Long term, children are at higher risk of being overweight and of developing type 2 diabetes.
Feline diabetes mellitus is a chronic disease in cats whereby either insufficient insulin response or insulin resistance leads to persistently high blood glucose concentrations. Diabetes affects up to 1 in 230 cats, and may be becoming increasingly common. Diabetes is less common in cats than in dogs. The condition is treatable, and if treated properly the cat can experience a normal life expectancy. In cats with type 2 diabetes, prompt effective treatment may lead to diabetic remission, in which the cat no longer needs injected insulin. Untreated, the condition leads to increasingly weak legs in cats and eventually to malnutrition, ketoacidosis and/or dehydration, and death.

Diabetic hypoglycemia is a low blood glucose level occurring in a person with diabetes mellitus. It is one of the most common types of hypoglycemia seen in emergency departments and hospitals. According to the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP), and based on a sample examined between 2004 and 2005, an estimated 55,819 cases involved insulin, and severe hypoglycemia is likely the single most common event.
The term diabetes includes several different metabolic disorders that all, if left untreated, result in abnormally high concentrations of a sugar called glucose in the blood. Diabetes mellitus type 1 results when the pancreas no longer produces significant amounts of the hormone insulin, usually owing to the autoimmune destruction of the insulin-producing beta cells of the pancreas. Diabetes mellitus type 2, in contrast, is now thought to result from autoimmune attacks on the pancreas and/or insulin resistance. The pancreas of a person with type 2 diabetes may be producing normal or even abnormally large amounts of insulin. Other forms of diabetes mellitus, such as the various forms of maturity-onset diabetes of the young, may represent some combination of insufficient insulin production and insulin resistance. Some degree of insulin resistance may also be present in a person with type 1 diabetes.
Many types of glucose tests exist and they can be used to estimate blood sugar levels at a given time or, over a longer period of time, to obtain average levels or to see how fast body is able to normalize changed glucose levels. Eating food for example leads to elevated blood sugar levels. In healthy people, these levels quickly return to normal via increased cellular glucose uptake which is primarily mediated by increase in blood insulin levels.

For pregnant women with diabetes, some particular challenges exist for both mother and fetus. If the pregnant woman has diabetes as a pre-existing disorder, it can cause early labor, birth defects, and larger than average infants. Therefore, experts advise diabetics to maintain blood sugar level close to normal range about 3 months before planning for pregnancy.
A diabetic diet is a diet that is used by people with diabetes mellitus or high blood sugar to minimize symptoms and dangerous complications of long-term elevations in blood sugar.
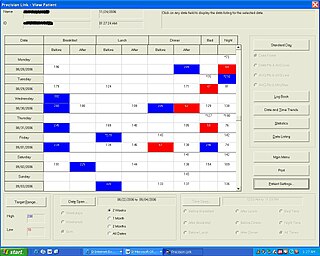
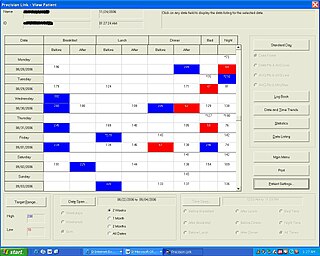
Diabetes Management Software refers to software tools that run on personal computers and personal digital assistants to help persons with Type 1 and Type 2 diabetes manage the data associated with:
Chronic Somogyi rebound is a contested explanation of phenomena of elevated blood sugars experienced by diabetics in the morning. Also called the Somogyi effect and posthypoglycemic hyperglycemia, it is a rebounding high blood sugar that is a response to low blood sugar. When managing the blood glucose level with insulin injections, this effect is counter-intuitive to people who experience high blood sugar in the morning as a result of an overabundance of insulin at night.

Prediabetes is a component of metabolic syndrome and is characterized by elevated blood sugar levels that fall below the threshold to diagnose diabetes mellitus. It usually does not cause symptoms but people with prediabetes often have obesity, dyslipidemia with high triglycerides and/or low HDL cholesterol, and hypertension. It is also associated with increased risk for cardiovascular disease (CVD). Prediabetes is more accurately considered an early stage of diabetes as health complications associated with type 2 diabetes often occur before the diagnosis of diabetes.

As a medication, insulin is any pharmaceutical preparation of the protein hormone insulin that is used to treat high blood glucose. Such conditions include type 1 diabetes, type 2 diabetes, gestational diabetes, and complications of diabetes such as diabetic ketoacidosis and hyperosmolar hyperglycemic states. Insulin is also used along with glucose to treat hyperkalemia. Typically it is given by injection under the skin, but some forms may also be used by injection into a vein or muscle. There are various types of insulin, suitable for various time spans. The types are often all called insulin in the broad sense, although in a more precise sense, insulin is identical to the naturally occurring molecule whereas insulin analogues have slightly different molecules that allow for modified time of action. It is on the World Health Organization's List of Essential Medicines. In 2021, it was the 179th most commonly prescribed medication in the United States, with more than 2 million prescriptions.

Diabetes mellitus, often known simply as diabetes, is a group of common endocrine diseases characterized by sustained high blood sugar levels. Diabetes is due to either the pancreas not producing enough insulin, or the cells of the body becoming unresponsive to the hormone's effects. Classic symptoms include thirst, polyuria, weight loss, and blurred vision. If left untreated, the disease can lead to various health complications, including disorders of the cardiovascular system, eye, kidney, and nerves. Diabetes accounts for approximately 4.2 million deaths every year, with an estimated 1.5 million caused by either untreated or poorly treated diabetes.