Blood transfusion is the process of transferring blood products into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, plasma, platelets, and other clotting factors. White blood cells are transfused only in very rare circumstances, since granulocyte transfusion has limited applications. Whole blood has come back into use in the trauma setting.

Blood plasma is a light amber-colored liquid component of blood in which blood cells are absent, but which contains proteins and other constituents of whole blood in suspension. It makes up about 55% of the body's total blood volume. It is the intravascular part of extracellular fluid. It is mostly water, and contains important dissolved proteins, glucose, clotting factors, electrolytes, hormones, carbon dioxide, and oxygen. It plays a vital role in an intravascular osmotic effect that keeps electrolyte concentration balanced and protects the body from infection and other blood-related disorders.

The Magen David Adom is Israel's national emergency medical, disaster, ambulance and blood bank service. The literal meaning of name is "Red Shield of David," but the symbol is more frequently called the "Red Star of David" in many languages. Since June 2006, Magen David Adom has been officially recognized by the International Committee of the Red Cross (ICRC) as the national aid society of the State of Israel under the Geneva Conventions, and a member of the International Federation of Red Cross and Red Crescent Societies. MDA has a dedicated medical emergency phone number in Israel, 101. MDA can become an auxiliary arm of the Israel Defense Forces during times of war. In 2022, MDA became academically affiliated with Ben-Gurion University of the Negev. Following the October 7th attacks against Israel, the American Red Cross presented Magen David Adom with the International Humanitarian Service Award stating that the organization "exemplifies and inspires the humanitarian values of human dignity, respect, [and] compassion."

A blood bank is a center where blood gathered as a result of blood donation is stored and preserved for later use in blood transfusion. The term "blood bank" typically refers to a department of a hospital usually within a clinical pathology laboratory where the storage of blood product occurs and where pre-transfusion and blood compatibility testing is performed. However, it sometimes refers to a collection center, and some hospitals also perform collection. Blood banking includes tasks related to blood collection, processing, testing, separation, and storage.

A blood donation occurs when a person voluntarily has blood drawn and used for transfusions and/or made into biopharmaceutical medications by a process called fractionation. A donation may be of whole blood, or of specific components directly (apheresis). Blood banks often participate in the collection process as well as the procedures that follow it.
The Canadian Red Cross Society is a Canadian humanitarian charitable organization, and one of 192 national Red Cross and Red Crescent societies. The organization receives funding from both private donations and from Canadian government departments.

Plasmapheresis is the removal, treatment, and return or exchange of blood plasma or components thereof from and to the blood circulation. It is thus an extracorporeal therapy, a medical procedure performed outside the body.

Plateletpheresis is the process of collecting thrombocytes, more commonly called platelets, a component of blood involved in blood clotting. The term specifically refers to the method of collecting the platelets, which is performed by a device used in blood donation that separates the platelets and returns other portions of the blood to the donor. Platelet transfusion can be a life-saving procedure in preventing or treating serious complications from bleeding and hemorrhage in patients who have disorders manifesting as thrombocytopenia or platelet dysfunction. This process may also be used therapeutically to treat disorders resulting in extraordinarily high platelet counts such as essential thrombocytosis.
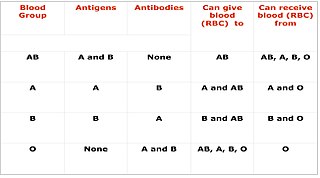
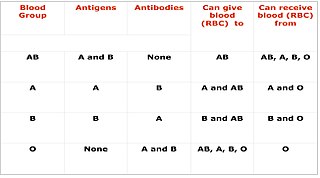
Cross-matching or crossmatching is a test performed before a blood transfusion as part of blood compatibility testing. Normally, this involves adding the recipient's blood plasma to a sample of the donor's red blood cells. If the blood is incompatible, the antibodies in the recipient's plasma will bind to antigens on the donor red blood cells. This antibody-antigen reaction can be detected through visible clumping or destruction of the red blood cells, or by reaction with anti-human globulin. Along with blood typing of the donor and recipient and screening for unexpected blood group antibodies, cross-matching is one of a series of steps in pre-transfusion testing. In some circumstances, an electronic cross-match can be performed by comparing records of the recipient's ABO and Rh blood type against that of the donor sample. In emergencies, blood may be issued before cross-matching is complete. Cross-matching is also used to determine compatibility between a donor and recipient in solid organ transplantation including heart/lung transplation.

In England, blood and other tissues are collected by NHS Blood and Transplant (NHSBT). NHSBT Blood Donation was previously known as the National Blood Service until it merged with UK Transplant in 2005 to form a NHS special health authority. Other official blood services in the United Kingdom include the Northern Ireland Blood Transfusion Service, the Scottish National Blood Transfusion Service and the Welsh Blood Service.
NHS Blood and Transplant is an executive special health authority of the United Kingdom's Department of Health and Social Care. It was established on 1 October 2005 to take over the responsibilities of two separate NHS agencies: UK Transplant, founded by Dr. Geoffrey Tovey in 1972, and the National Blood Service. Its remit is to provide a reliable, efficient supply of blood, organs and associated services to the NHS. Since NHSBT was established, the organisation has maintained or improved the quality of the services delivered to patients, stabilised the rising cost of blood, and centralised a number of corporate services.
The New Zealand Blood Service is the provider of blood services for New Zealand. The service is a Crown entity responsible to New Zealand's Parliament and is governed by a Board appointed by the Minister of Health.
Many countries have laws, regulations, or recommendations that effectively prohibit donations of blood or tissue for organ and corneal transplants from men who have sex with men (MSM), a classification irrespective of their sexual activities with same-sex partners and of whether they identify themselves as bisexual or gay. Temporary restrictions are sometimes called "deferrals", since blood donors who are found ineligible may be found eligible at a later date. However, many deferrals are indefinite meaning that donations are not accepted at any point in the future, constituting a de facto ban. Even men who have monogamous relations with their same-sex partners are found ineligible.

The Associazione Volontari Italiani del Sangue (AVIS) is the major Italian non-profit and charitable organisation for blood donation, bringing together over a million volunteer blood donors across Italy. It is headquartered in Lombardy, Italy.

The South African National Blood Service (SANBS) is a non-profit organisation that provides human blood for transfusion that operates in South Africa, with the exception of the Western Cape, which has its own blood service. The head office of the SANBS is in Constantia Kloof, Gauteng, near Johannesburg, but there are blood collection operations in eight of the nine provinces. Western Cape has a separate blood centre, the Western Cape Blood Service. SANBS was founded in 2001 from a merger of seven blood centres, and was embroiled in controversy in 2004 over a policy of racial profiling for blood safety.
Blood donation in Bangladesh is an activity conducted by several different organisations. As of 2011, about 25% of the nation's blood supply came from voluntary donation, 20–25% from paid donors, and 50–55% from one-time donation for a specific patient.

Frederic Duran i Jordà was a Catalan medical doctor, pioneer hematology and hemotherapy. He created the first transfusion service in the world in Barcelona in 1936 at the beginning of the Spanish Civil War. Previously there were blood banks, where donated blood to be transfused was stored. Dr. Duran i Jordà created a methodology that would serve to collect massive blood donations and be transfused distance, in this case the front lines of the Spanish Civil War. This method was subsequently applied in World War II.

American Red Cross Motor Corps was founded in 1917 by the American Red Cross (ARC). The service was composed of women and it was developed to render supplementary aid to the U.S. Army and Navy in transporting troops and supplies during World War I, and to assist other ARC workers in conducting their various relief activities. The diverse character of the work included canteen work, military hospitals, camps and cantonments, home service workers, outside aid, office detail, other ARC activities, and miscellaneous services, such as the 1918 flu pandemic.
Blood donations in India are conducted by organisations and hospitals through blood donation camps. Donors can also visit blood banks in hospitals to donate blood. Efforts by the government and advocacy groups over the years have helped bridge the gap between demand and supply. The regulatory framework for blood donation and blood bank management rests with the Central Drugs Standard Control Organisation, while technical bodies like the National Blood Transfusion Council and National AIDS Control Organisation formulate guidelines and recommendations for transfusion medicine and blood bank management. Challenges persist with regards to regulation of blood banks and transfusion practices as the sector is largely fragmented with uneven distribution of blood banks and supply of blood in parts of the country. Donors are usually provided with refreshments after the procedure, which include glucose drinks, biscuits and fruits. Some organisations offer transportation facilities, as well as certificates or badges as gratitude.
The San Diego Blood Sisters were a group who sponsored and organized lesbian blood drives during the AIDS epidemic. Established by members of the Women's Caucus of the San Diego Democratic Club, the Blood Sisters sought to gather an adequate blood supply for AIDS patients, primarily gay men who often required many transfusions due to anemia. The organization's history ranges from their formation in 1983 to their slow dissolution after President Ronald Reagan's eventual intervention in the epidemic. The Blood Sisters' efforts were often contested, disrupted, or cancelled by those concerned for the safety of the blood supply.