Related Research Articles
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.
The spread of HIV/AIDS has affected millions of people worldwide; AIDS is considered a pandemic. The World Health Organization (WHO) estimated that in 2016 there were 36.7 million people worldwide living with HIV/AIDS, with 1.8 million new HIV infections per year and 1 million deaths due to AIDS. Misconceptions about HIV and AIDS arise from several different sources, from simple ignorance and misunderstandings about scientific knowledge regarding HIV infections and the cause of AIDS to misinformation propagated by individuals and groups with ideological stances that deny a causative relationship between HIV infection and the development of AIDS. Below is a list and explanations of some common misconceptions and their rebuttals.

Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When the brain is infected, symptoms include headache, fever, neck pain, nausea and vomiting, light sensitivity and confusion or changes in behavior. It can also affect other parts of the body including skin, where it may appear as several fluid-filled nodules with dead tissue.
Post-exposure prophylaxis, also known as post-exposure prevention (PEP), is any preventive medical treatment started after exposure to a pathogen in order to prevent the infection from occurring.

Nevirapine (NVP), sold under the brand name Viramune among others, is a medication used to treat and prevent HIV/AIDS, specifically HIV-1. It is generally recommended for use with other antiretroviral medications. It may be used to prevent mother to child spread during birth but is not recommended following other exposures. It is taken by mouth.
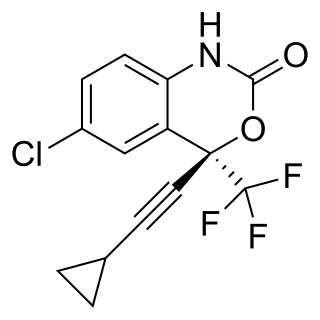
Efavirenz (EFV), sold under the brand names Sustiva among others, is an antiretroviral medication used to treat and prevent HIV/AIDS. It is generally recommended for use with other antiretrovirals. It may be used for prevention after a needlestick injury or other potential exposure. It is sold both by itself and in combination as efavirenz/emtricitabine/tenofovir. It is taken by mouth.

An opportunistic infection is an infection caused by pathogens that take advantage of an opportunity not normally available. These opportunities can stem from a variety of sources, such as a weakened immune system, an altered microbiome, or breached integumentary barriers. Many of these pathogens do not necessarily cause disease in a healthy host that has a non-compromised immune system, and can, in some cases, act as commensals until the balance of the immune system is disrupted. Opportunistic infections can also be attributed to pathogens which cause mild illness in healthy individuals but lead to more serious illness when given the opportunity to take advantage of an immunocompromised host.

Emtricitabine/tenofovir, sold under the brand name Truvada among others, is a fixed-dose combination antiretroviral medication used to treat and prevent HIV/AIDS. It contains the antiretroviral medications emtricitabine and tenofovir disoproxil. For treatment, it must be used in combination with other antiretroviral medications. For prevention before exposure, in those who are at high risk, it is recommended along with safer sex practices. It does not cure HIV/AIDS. Emtricitabine/tenofovir is taken by mouth.

The human immunodeficiency virus (HIV) is a retrovirus that attacks the immune system. It can be managed with treatment. Without treatment it can lead to a spectrum of conditions including acquired immunodeficiency syndrome (AIDS).

Pre-exposure prophylaxis for HIV prevention, commonly known as PrEP, is a form of medication used to prevent HIV infection, the cause of HIV/AIDS.

HIV/AIDS was first detected in Canada in 1982. In 2018, there were approximately 62,050 people living with HIV/AIDS in Canada. It was estimated that 8,300 people were living with undiagnosed HIV in 2018. Mortality has decreased due to medical advances against HIV/AIDS, especially highly active antiretroviral therapy (HAART).
Michael (Mike) Simon Youle is a British doctor and clinical researcher specializing in HIV treatment. He publicised the concept of pre-exposure prophylaxis (PREP) for HIV and has studied the health economics of HIV therapy. In 1995, he was listed as one of 40 influential gay men by The Independent.
HIV prevention refers to practices that aim to prevent the spread of the human immunodeficiency virus (HIV). HIV prevention practices may be undertaken by individuals to protect their own health and the health of those in their community, or may be instituted by governments and community-based organizations as public health policies.

HIV/AIDS research includes all medical research that attempts to prevent, treat, or cure HIV/AIDS, as well as fundamental research about the nature of HIV as an infectious agent and AIDS as the disease caused by HIV.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.
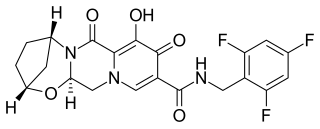
Bictegravir is a second-generation integrase inhibitor (INSTI) class that was structurally derived from an earlier compound dolutegravir by scientists at Gilead Sciences. In vitro and clinical results were presented by Gilead in the summer of 2016. In 2016, bictegravir was in a Phase 3 trial as part of a single tablet regimen in combination with tenofovir alafenamide (TAF) and emtricitabine (FTC) for the treatment of HIV-1 infection.

Bictegravir/emtricitabine/tenofovir alafenamide, sold under the brand name Biktarvy, is a fixed-dose combination antiretroviral medication for the treatment of HIV/AIDS. One tablet, taken orally once daily, contains 50 mg bictegravir, 200 mg emtricitabine, and 25 mg tenofovir alafenamide.
Laura Jane Waters is a British physician, genitourinary consultant at the National Health Service (NHS) Mortimer Market Centre in London. She was chair of the British HIV Association (BHIVA) until 2023 and advises the NHS on HIV treatment. Waters is a regular contributor to Boyz magazine, and throughout the COVID-19 pandemic provided regular advice to HIV-positive people.

Chloe Meave Orkin is a British physician and Professor of HIV/AIDS medicine at Queen Mary University of London. She works as a consultant at the Royal London Hospital, Barts Health NHS Trust. She is an internationally renowned expert in HIV therapeutics and led the first phase III clinical trial of injectable anti-retrovirals. She is immediate past Chair of the British HIV Association, where she championed the Undetectable=Untransmittable (U=U) campaign within the United Kingdom. She is president elect of the Medical Women's Federation. Orkin is gay and was on the Top 100 Lesbian influencer lists in both the UK and in the US in 2020. She considers herself a medical activist and much of her work focuses on inequalities in healthcare and in Medicine.
Margaret Johnson is a British physician who is a consultant in thoracic medicine and chair of the St John & St Elizabeth Hospital. In the late 1980s, she was the first dedicated HIV doctor at the Royal Free Hospital.
References
- ↑ "Executive Committee". www.bhiva.org. Retrieved 2020-04-19.
- ↑ Orkin, Chloe. "Kings Fund Concluding Remarks" (PDF). www.kingsfund.org.uk. Retrieved 12 September 2017.
- ↑ i-base (12 September 2017). "i-base Future Meetings". i-base.
- ↑ NICE (12 September 2017). "NICE Accreditation Decisions".
- ↑ Brady, Michael; et al. (14 March 2019). "BHIVA/BASHH guidelines on the use of HIV pre–exposure prophylaxis (PrEP) 2018". HIV Medicine. 20 (S2): s2–s80. doi: 10.1111/hiv.12718 . PMID 30869189.
- ↑ Churchill, Duncan; et al. (17 Aug 2016). "British HIV Association guidelines for the treatment of HIV-1-positive adults with antiretroviral therapy 2015" (PDF). HIV Medicine. 17 (s4): s2–s104. doi:10.1111/hiv.12426. PMID 27568911. S2CID 32394203.
- ↑ Geretti, AM; et al. (17 Aug 2016). "British HIV Association Guidelines on the Use of Vaccines in HIV-Positive Adults 2015" (PDF). HIV Medicine. 17 (s3): s2–s81. doi:10.1111/hiv.12424. PMID 27568789. S2CID 142893.
- ↑ Cresswell, Fiona; et al. (27 Aug 2016). "UK guideline for the use of HIV Post-Exposure Prophylaxis Following Sexual Exposure, 2015" (PDF). Int J STD AIDS. 27 (9): 713–38. doi:10.1177/0956462416641813. PMID 27095790. S2CID 33255206.
- ↑ Nelson, M; et al. (Sep 2011). "British HIV Association and British Infection Association guidelines for the treatment of opportunistic infection in HIV-seropositive individuals 2011". HIV Medicine. 12 (S2): 1–140. doi: 10.1111/j.1468-1293.2011.00944_1.x . PMID 21851517. S2CID 22513510.