Related Research Articles

A blood type is a classification of blood, based on the presence and absence of antibodies and inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system. Some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens can stem from one allele and collectively form a blood group system.

Blood transfusion is the process of transferring blood products into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, plasma, platelets, and other clotting factors. White blood cells are transfused only in very rare circumstances, since granulocyte transfusion has limited applications. Whole blood has come back into use in the trauma setting.

Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location. Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source.

Charles Richard Drew was an American surgeon and medical researcher. He researched in the field of blood transfusions, developing improved techniques for blood storage, and applied his expert knowledge to developing large-scale blood banks early in World War II. This allowed medics to save thousands of Allied forces' lives during the war. As the most prominent African American in the field, Drew protested against the practice of racial segregation in the donation of blood, as it lacked scientific foundation, and resigned his position with the American Red Cross, which maintained the policy until 1950.

Michael Ellis DeBakey was an American general and cardiovascular surgeon, scientist and medical educator who became Chairman of the Department of Surgery, President, and Chancellor of Baylor College of Medicine at the Texas Medical Center in Houston, Texas. His career spanned nearly eight decades.

A blood bank is a center where blood gathered as a result of blood donation is stored and preserved for later use in blood transfusion. The term "blood bank" typically refers to a department of a hospital usually within a clinical pathology laboratory where the storage of blood product occurs and where pre-transfusion and blood compatibility testing is performed. However, it sometimes refers to a collection center, and some hospitals also perform collection. Blood banking includes tasks related to blood collection, processing, testing, separation, and storage.

A blood donation occurs when a person voluntarily has blood drawn and used for transfusions and/or made into biopharmaceutical medications by a process called fractionation. A donation may be of whole blood, or of specific components directly (apheresis). Blood banks often participate in the collection process as well as the procedures that follow it.

Liver transplantation or hepatic transplantation is the replacement of a diseased liver with the healthy liver from another person (allograft). Liver transplantation is a treatment option for end-stage liver disease and acute liver failure, although availability of donor organs is a major limitation. Liver transplantation is highly regulated, and only performed at designated transplant medical centers by highly trained transplant physicians. Favorable outcomes require careful screening for eligible recipients, as well as a well-calibrated live or deceased donor match.
Serology is the scientific study of serum and other body fluids. In practice, the term usually refers to the diagnostic identification of antibodies in the serum. Such antibodies are typically formed in response to an infection, against other foreign proteins, or to one's own proteins. In either case, the procedure is simple.
Cord blood is blood that remains in the placenta and in the attached umbilical cord after childbirth. Cord blood is collected because it contains stem cells, which can be used to treat hematopoietic and genetic disorders such as cancer.

Bernard Fantus was a Hungarian Jewish-American physician. He established the first hospital blood bank in the United States in 1937 at Cook County Hospital, Chicago while he served there as director of the pharmacology and therapeutics department.

Arterial switch operation (ASO) or arterial switch, is an open heart surgical procedure used to correct dextro-transposition of the great arteries (d-TGA).
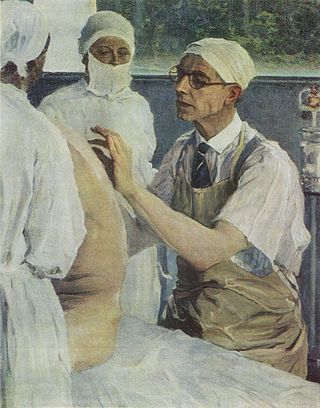
Sergei Sergeevich Yudin was a Russian surgeon.
Yudin/Judin (male) and Yudina/Judina (female) are Russian surnames derived from the name Yuda, a Russified version of the former calendar name Jude, no longer in use. In Belarus and Western Ukraine the origin might be the name Judith. Also adopted by Jews following the Partitions of Poland, in reference to a village name Yudino or meaning "the son/daughter of Jude".

Karl Landsteiner was an Austrian-American biologist, physician, and immunologist. He emigrated with his family to New York in 1923 at the age of 55 for professional opportunities, working for the Rockefeller Institute.

Frederic Duran i Jordà was a Catalan medical doctor, pioneer hematology and hemotherapy. He created the first transfusion service in the world in Barcelona in 1936 at the beginning of the Spanish Civil War. Previously there were blood banks, where donated blood to be transfused was stored. Dr. Duran i Jordà created a methodology that would serve to collect massive blood donations and be transfused distance, in this case the front lines of the Spanish Civil War. This method was subsequently applied in World War II.
Richard Lewisohn was a German-American surgeon. At Mount Sinai Hospital in Manhattan, he developed procedures that made blood transfusion practical.

Charles Granville Rob was a British surgeon who pioneered techniques in the repair of damaged blood vessels, particularly the operation to unblock arteries of the neck, known as carotid endarterectomy and of the aorta when treating aortic aneurysms.
The 2020 Nobel Prize in Physiology or Medicine was awarded to the American virologists Harvey J. Alter, Michael Houghton and Charles M. Rice "for the discovery of Hepatitis C virus." During the award ceremony on December 10, 2020, Prof. Gunilla Karlsson-Hedestam said:
"The discovery of the Hepatitis C virus by this year’s Laureates laid the foundation for our current understanding about how the virus survives in its niche during the long chronic phase of the infection, and how liver disease develops. And importantly, it led to the development of highly effective anti-viral medicines that now cure the infection in almost all treated persons."
References
- ↑ (Robert A. Kilduffe and Michael DeBakey, 1942)
- Shamov VN and Kostriukov M. Questions of homoplasty from the cadaver. Blood transfusion from cadaver, Trudi Ukrain. Suezda. Khir. 1929;18:184.
- Shamov WN. The transfusion of stored cadaver blood Lancet 1937; 2, August 7:306–309
- Judine S. La transfusion du sang de cadavre á l'homme. Paris: Masson et Cie, 1933.
- Yudin S. Transfusion of stored cadaver blood. Practical consideration: The first thousand cases. Lancet 1937;2:361–366.
- Yudin S. Transfusion of cadaver blood. JAMA 1936;106:997–999.
- Swan H, Schechter D. The transfusion of blood from cadavers. A historical review. Surgery 1962;52:545.
- Kilduffe R, DeBakey M. The blood bank and the technique and therapeutics of transfusion. St. Louis: The C.V.Mosby Company, 1942, pp. 196–197
- Kevorkian J, Marra JJ. Transfusion of Human Corps Blood without Additives.Transfusion. 1964;4:112–117.