Physiology
| | This section is empty. You can help by adding to it. (August 2024) |
| Carbohydrate-deficient transferrin | |
|---|---|
| LOINC | 12949-4, 13999-8 |
Carbohydrate-deficient transferrin (CDT, also known as desialotransferrin or asialotransferrin) is a laboratory test used to help detect heavy ethanol consumption. [1]
| | This section is empty. You can help by adding to it. (August 2024) |
Carbohydrate-deficient transferrin is elevated in the blood of people with heavy alcohol consumption but elevated levels can also be found in a number of medical conditions. The limitations of the assay depend upon the methodology of the test. HPLC (High Performance Liquid Chromatography) can detect certain genetic variants and potential liver diseases affecting CDT.
Used with other tests, such as gamma glutamyl transferase (GGT), aspartate aminotransferase (AST), and alanine aminotransferase (ALT), carbohydrate-deficient transferrin can be a useful tool in identifying problem drinking, such as alcohol use disorder. However, it is less sensitive than phosphatidylethanol (PEth) in detecting current regular alcohol consumption.
The ethanol conjugates called ethyl glucuronide and ethyl sulfate remain detectable for up to three days after ethanol consumption and are quite useful for detection of occult/denied alcohol use disorder. Both these substances are detectable clinically through urine drug testing by commercial toxicology labs. [2]
CDT is measured by taking a sample of a patient's blood. Apparently healthy individuals with no or low reported alcohol consumption and a negative Alcohol Use Disorders Identification Test (AUDIT) will have a %CDT <1.7% (95th percentile for the social drinking population). Elevated levels of CDT suggest recent heavy alcohol consumption, especially if other liver-associated enzymes (such as GGT) are elevated. Although recent heavy alcohol use is most commonly associated with elevated CDT, certain rare liver disorders can also increase levels of CDT. CDT levels are less useful for detecting alcohol use disorder in people with other liver diseases. [3]

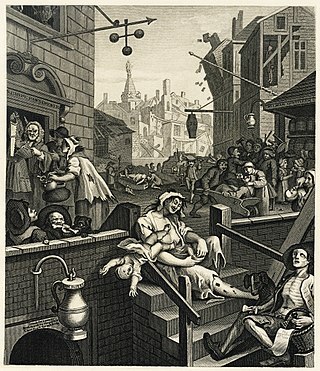
Alcoholism is the continued drinking of alcohol despite it causing problems. Some definitions require evidence of dependence and withdrawal. Problematic use of alcohol has been mentioned in the earliest historical records. The World Health Organization (WHO) estimated there were 283 million people with alcohol use disorders worldwide as of 2016. The term alcoholism was first coined in 1852, but alcoholism and alcoholic are sometimes considered stigmatizing and to discourage seeking treatment, so diagnostic terms such as alcohol use disorder or alcohol dependence are often used instead in a clinical context.
Liver function tests, also referred to as a hepatic panel, are groups of blood tests that provide information about the state of a patient's liver. These tests include prothrombin time (PT/INR), activated partial thromboplastin time (aPTT), albumin, bilirubin, and others. The liver transaminases aspartate transaminase and alanine transaminase are useful biomarkers of liver injury in a patient with some degree of intact liver function.
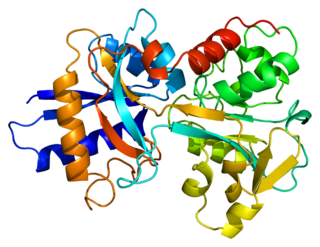
Alanine transaminase (ALT), also known as alanine aminotransferase, formerly serum glutamate-pyruvate transaminase (GPT) or serum glutamic-pyruvic transaminase (SGPT), is a transaminase enzyme that was first characterized in the mid-1950s by Arthur Karmen and colleagues. ALT is found in plasma and in various body tissues but is most common in the liver. It catalyzes the two parts of the alanine cycle. Serum ALT level, serum AST level, and their ratio are routinely measured clinically as biomarkers for liver health.

Alcoholic liver disease (ALD), also called alcohol-related liver disease (ARLD), is a term that encompasses the liver manifestations of alcohol overconsumption, including fatty liver, alcoholic hepatitis, and chronic hepatitis with liver fibrosis or cirrhosis.

Wernicke-Korsakoff syndrome (WKS) is the combined presence of Wernicke encephalopathy (WE) and alcoholic Korsakoff syndrome. Due to the close relationship between these two disorders, people with either are usually diagnosed with WKS as a single syndrome. It mainly causes vision changes, ataxia and impaired memory.
The long-term effects of alcohol have been extensively researched. The health effects of long-term alcohol consumption on health vary depending on the amount consumed. Even light drinking poses health risks, but atypically small amounts of alcohol may have health benefits. Alcoholism causes severe health consequences which outweigh any potential benefits.

Gamma-glutamyltransferase is a transferase that catalyzes the transfer of gamma-glutamyl functional groups from molecules such as glutathione to an acceptor that may be an amino acid, a peptide or water. GGT plays a key role in the gamma-glutamyl cycle, a pathway for the synthesis and degradation of glutathione as well as drug and xenobiotic detoxification. Other lines of evidence indicate that GGT can also exert a pro-oxidant role, with regulatory effects at various levels in cellular signal transduction and cellular pathophysiology. This transferase is found in many tissues, the most notable one being the liver, and has significance in medicine as a diagnostic marker.
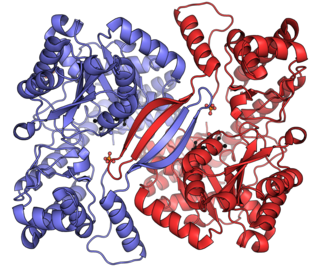
Transferrins are glycoproteins found in vertebrates which bind and consequently mediate the transport of iron (Fe) through blood plasma. They are produced in the liver and contain binding sites for two Fe3+ ions. Human transferrin is encoded by the TF gene and produced as a 76 kDa glycoprotein.

Alcoholic hepatitis is hepatitis due to excessive intake of alcohol. Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8–10 drinks per day. It is usually found in association with fatty liver, an early stage of alcoholic liver disease, and may contribute to the progression of fibrosis, leading to cirrhosis. Symptoms may present acutely after a large amount of alcoholic intake in a short time period, or after years of excess alcohol intake. Signs and symptoms of alcoholic hepatitis include jaundice, ascites, fatigue and hepatic encephalopathy. Mild cases are self-limiting, but severe cases have a high risk of death. Severity in alcoholic hepatitis is determined several clinical prediction models such as the Maddrey's Discriminant Function and the MELD score.

Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.
Alcohol tolerance refers to the bodily responses to the functional effects of ethanol. This includes direct tolerance, speed of recovery from insobriety and resistance to the development of alcohol use disorder.
Alcohol has a number of effects on health. Short-term effects of alcohol consumption include intoxication and dehydration. Long-term effects of alcohol include changes in the metabolism of the liver and brain, with increased risk of several types of cancer and alcohol use disorder. Alcohol intoxication affects the brain, causing slurred speech, clumsiness, and delayed reflexes. There is an increased risk of developing an alcohol use disorder for teenagers while their brain is still developing. Adolescents who drink have a higher probability of injury including death.
In medicine, the presence of elevated transaminases, commonly the transaminases alanine transaminase (ALT) and aspartate transaminase (AST), may be an indicator of liver dysfunction. Other terms include transaminasemia, and elevatedliver enzymes. Normal ranges for both ALT and AST vary by gender, age, and geography and are roughly 8-40 U/L. Mild transaminesemia refers to levels up to 250 U/L. Drug-induced increases such as that found with the use of anti-tuberculosis agents such as isoniazid are limited typically to below 100 U/L for either ALT or AST. Muscle sources of the enzymes, such as intense exercise, are unrelated to liver function and can markedly increase AST and ALT. Cirrhosis of the liver or fulminant liver failure secondary to hepatitis commonly reach values for both ALT and AST in the >1000 U/L range; however, many people with liver disease have normal transaminases. Elevated transaminases that persist less than six months are termed "acute" in nature, and those values that persist for six months or more are termed "chronic" in nature.
The AST/ALT ratio or De Ritis ratio is the ratio between the concentrations of two enzymes, aspartate transaminase (AST) and alanine transaminase, aka alanine aminotransferase (ALT), in the blood of a human or animal. It is used as one of several liver function tests, and measured with a blood test. It is sometimes useful in medical diagnosis for elevated transaminases to differentiate between causes of liver damage, or hepatotoxicity.

Ethyl glucuronide (EtG) is a metabolite of ethanol which is formed in the body by glucuronidation following exposure to ethanol, usually from drinking alcoholic beverages. It is used as a biomarker to test for ethanol use and to monitor alcohol abstinence in situations where drinking is prohibited, such as by the military, in alcohol treatment programs, in professional monitoring programs, in schools, liver transplant clinics, or in recovering alcoholic patients. In addition to its use to monitor abstinence and detect drinking, EtG also has potential for monitoring the amount of alcohol use over time because it can be detected in hair and nails, though the effectiveness of this has not yet been proven.

Phosphatidylethanols (PEth) are a group of phospholipids formed only in the presence of ethanol via the action of phospholipase D (PLD). It accumulates in blood and is removed slowly, making it a useful biomarker for alcohol consumption. PEth is also thought to contribute to the symptoms of alcohol intoxication.
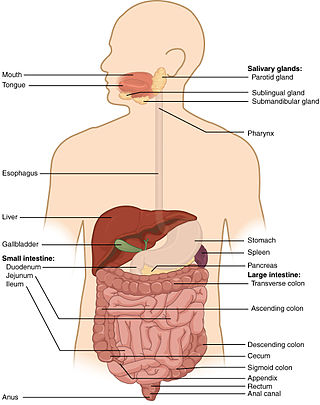
Auto-brewery syndrome (ABS) is a condition characterized by the fermentation of ingested carbohydrates in the gastrointestinal tract of the body caused by bacteria or fungi. ABS is a rare medical condition in which intoxicating quantities of ethanol are produced through endogenous fermentation within the digestive system. The organisms responsible for ABS include various yeasts and bacteria, including Saccharomyces cerevisiae, S. boulardii, Candida albicans, C. tropicalis, C. krusei, C. glabrata, C. parapsilosis, Kluyveromyces marxianus, Klebsiella pneumoniae, and Enterococcus faecium. These organisms use lactic acid fermentation or mixed acid fermentation pathways to produce an ethanol end product. The ethanol generated from these pathways is absorbed in the small intestine, causing an increase in blood alcohol concentrations that produce the effects of intoxication without the consumption of alcohol.

Alcohol, sometimes referred to by the chemical name ethanol, is the second most consumed psychoactive drug globally behind caffeine, and alcohol use disorders are the most prevalent of all substance use disorders worldwide. Alcohol is a central nervous system (CNS) depressant, decreasing electrical activity of neurons in the brain. The World Health Organization (WHO) classifies alcohol as a toxic, psychoactive, dependence-producing, and carcinogenic substance.
Alcohol-related brain damage alters both the structure and function of the brain as a result of the direct neurotoxic effects of alcohol intoxication or acute alcohol withdrawal. Increased alcohol intake is associated with damage to brain regions including the frontal lobe, limbic system, and cerebellum, with widespread cerebral atrophy, or brain shrinkage caused by neuron degeneration. This damage can be seen on neuroimaging scans.

Alcohol intolerance is due to a genetic polymorphism of the aldehyde dehydrogenase enzyme, which is responsible for the metabolism of acetaldehyde. This polymorphism is most often reported in patients of East Asian descent. Alcohol intolerance may also be an associated side effect of certain drugs such as disulfiram, metronidazole, or nilutamide. Skin flushing and nasal congestion are the most common symptoms of intolerance after alcohol ingestion. It may also be characterized as intolerance causing hangover symptoms similar to the "disulfiram-like reaction" of aldehyde dehydrogenase deficiency or chronic fatigue syndrome. Severe pain after drinking alcohol may indicate a more serious underlying condition.