Related Research Articles

Organ donation is the process when a person authorizes an organ of their own to be removed and transplanted to another person, legally, either by consent while the donor is alive, through a legal authorization for deceased donation made prior to death, or for deceased donations through the authorization by the legal next of kin.

Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location. Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source.
Bioethics is both a field of study and professional practice, interested in ethical issues related to health, including those emerging from advances in biology, medicine, and technologies. It proposes the discussion about moral discernment in society and it is often related to medical policy and practice, but also to broader questions as environment, well-being and public health. Bioethics is concerned with the ethical questions that arise in the relationships among life sciences, biotechnology, medicine, politics, law, theology and philosophy. It includes the study of values relating to primary care, other branches of medicine, ethical education in science, animal, and environmental ethics, and public health.
Medical ethics is an applied branch of ethics which analyzes the practice of clinical medicine and related scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. These values include the respect for autonomy, non-maleficence, beneficence, and justice. Such tenets may allow doctors, care providers, and families to create a treatment plan and work towards the same common goal. These four values are not ranked in order of importance or relevance and they all encompass values pertaining to medical ethics. However, a conflict may arise leading to the need for hierarchy in an ethical system, such that some moral elements overrule others with the purpose of applying the best moral judgement to a difficult medical situation. Medical ethics is particularly relevant in decisions regarding involuntary treatment and involuntary commitment.
Prior to the introduction of brain death into law in the mid to late 1970s, all organ transplants from cadaveric donors came from non-heart-beating donors (NHBDs).

Xenotransplantation, or heterologous transplant, is the transplantation of living cells, tissues or organs from one species to another. Such cells, tissues or organs are called xenografts or xenotransplants. It is contrasted with allotransplantation, syngeneic transplantation or isotransplantation and autotransplantation. Xenotransplantation is an artificial method of creating an animal-human chimera, that is, a human with a subset of animal cells. In contrast, an individual where each cell contains genetic material from a human and an animal is called a human–animal hybrid.
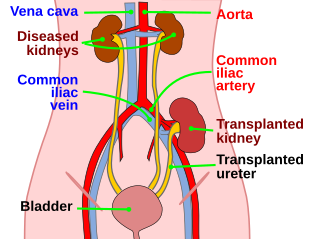
Kidney transplant or renal transplant is the organ transplant of a kidney into a patient with end-stage kidney disease (ESRD). Kidney transplant is typically classified as deceased-donor or living-donor transplantation depending on the source of the donor organ. Living-donor kidney transplants are further characterized as genetically related (living-related) or non-related (living-unrelated) transplants, depending on whether a biological relationship exists between the donor and recipient. The first successful kidney transplant was performed in 1954 by a team including Joseph Murray, the recipient's surgeon, and Hartwell Harrison, surgeon for the donor. Murray was awarded a Nobel Prize in Physiology or Medicine in 1990 for this and other work. In 2018, an estimated 95,479 kidney transplants were performed worldwide, 36% of which came from living donors.

Ezekiel Jonathan "Zeke" Emanuel is an American oncologist, bioethicist and senior fellow at the Center for American Progress. He is the current Vice Provost for Global Initiatives at the University of Pennsylvania and chair of the Department of Medical Ethics and Health Policy. Previously, Emanuel served as the Diane and Robert Levy University Professor at Penn. He holds a joint appointment at the University of Pennsylvania School of Medicine and the Wharton School and was formerly an associate professor at the Harvard Medical School until 1998 when he joined the National Institutes of Health.
Organ procurement is a surgical procedure that removes organs or tissues for reuse, typically for organ transplantation.

The National Organ Transplant Act (NOTA) of 1984 is an Act of the United States Congress that created the framework for the organ transplant system in the country. The act provided clarity on the property rights of human organs obtained from deceased individuals and established a public-private partnership known as Organ Procurement and Transplantation Network (OPTN). The OPTN was given the authority to oversee the national distribution of organs.

Sigrid Fry-Revere is an American medical ethicist and lawyer who has worked on many issues in patient care ethics, but most recently has been working on the rights of living organ donors.
Organ trade is the trading of human organs, tissues, or other body products, usually for transplantation. According to the World Health Organization (WHO), organ trade is a commercial transplantation where there is a profit, or transplantations that occur outside of national medical systems. There is a global need or demand for healthy body parts for transplantation, which exceeds the numbers available.
The Nuffield Council on Bioethics is a UK-based independent charitable body, which examines and reports on bioethical issues raised by new advances in biological and medical research. Established in 1991, the Council is funded by the Nuffield Foundation, the Medical Research Council and the Wellcome Trust. The Council has been described by the media as a 'leading ethics watchdog', which 'never shrinks from the unthinkable'.
Many different major religious groups and denominations have varying views on organ donation of a deceased and live bodies, depending on their ideologies. Differing opinions can arise depending on if the death is categorized as brain death or cease of the heartbeat. It is important for doctors and health care providers to be knowledgeable about differentiating theological and cultural views on death and organ donations as nations are becoming more multicultural.

I. Glenn Cohen is a Canadian legal scholar and professor at Harvard Law School. He is also the director of Harvard Law School's Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics.

The practice of selling one's kidney for profit in Iran is legal and regulated by the government. In any given year, it is estimated that 1400 Iranians sell one of their kidneys to a recipient who was previously unknown to them. Iran currently is the only country in the world that allows the sale of one's kidney for compensation ; consequently, the country does not have either a waiting list or a shortage of available organs.
The MacLean Center for Clinical Medical Ethics, founded in 1981, is a non-profit clinical medical ethics research institute based in the United States. Founded by its director, Mark Siegler, the MacLean Center for Clinical Medical Ethics aims to improve patient care and outcomes by promoting research in clinical medical ethics by educating physicians, nurses, and other health care professionals and by helping University of Chicago Medicine patients, families, and health care providers identify and resolve ethical dilemmas. The center has trained over 410 fellows, including many physicians, attorneys, PhDs and bioethicists.
In bioethics, ethics of organ transplantation refers to the ethical concerns on organ transplantation procedures. Both the source and method of obtaining the organ to transplant are major ethical issues to consider, as well as the notion of distributive justice.
Organ donation in the United States prison population is the donation of biological tissues or organs from incarcerated individuals to living recipients in need of a transplantation.
Transplant coordinator is a healthcare professional – doctor, nurse, or allied health science graduate – who coordinates activities related to organ donation and transplantation. Transplant coordinators can either be Donor Coordinators or Recipient Coordinators.
References
- 1 2 "Center for Ethical Solutions, Inc" (PDF). Foundation Center. Retrieved 17 May 2017.
- 1 2 Ghods, Ahad J., and Shekoufeh Savaj. 2006. Iranian Model of Paid and Regulated Living-Unrelated Kidney Donation. Clin J Am Soc Nephrol 1, no. 6 (November 1): 1136-1145. doi : 10.2215/CJN.00700206.
- ↑ Griffin, Anne. 2007. Kidneys on demand. BMJ 334, no. 7592 (March 10): 502-505. doi : 10.1136/bmj.39141.493148.94.
- ↑ Gil-Díaz, Carlos. 2009. Spain's Record Organ Donations: Mining Moral Conviction. Cambridge Quarterly of Healthcare Ethics 18, no. 03: 256-261. doi : 10.1017/S0963180109090410.
- ↑ "The Spanish Model Archived June 6, 2008, at the Wayback Machine ". Organización Nacional de Trasplantes. Retrieved 2009-06-30.
- ↑ UK Organ donation taskforce report The potential impact of an opt out system for organ donation in the UK, page 22.
- ↑ The Associated Press (2004-06-30). 1 in 8 returning soldiers suffers from PTSD. NBC News. Retrieved on 2009-07-06.
- ↑ Taken from CATO-at-Liberty blog. http://www.cato-at-liberty.org/2007/09/23/legal-trends-in-bioethics/ Archived 2009-08-15 at the Wayback Machine Accessed 31 August 2009.
- ↑ Lloyd, Christopher (2009-02-02). Entrepreneurs pursuing patient advocacy trend. AllBusiness. Retrieved on 2009-07-06.