Related Research Articles

Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver.
Crohn's disease is a chronic inflammatory bowel disease characterized by recurrent episodes of intestinal inflammation, primarily manifesting as diarrhea and abdominal pain. Unlike ulcerative colitis, inflammation can occur anywhere in the gastrointestinal tract, though it most frequently affects the ileum and colon, involving all layers of the intestinal wall. Symptoms may be non-specific and progress gradually, often delaying diagnosis. About one-third of patients have colonic disease, another third have ileocolic disease, and the remaining third have isolated ileal disease. Systemic symptoms such as chronic fatigue, weight loss, and low-grade fevers are common. Organs such as the skin and joints can also be affected. Complications can include bowel obstructions, fistulas, nutrition problems, and an increased risk of intestinal cancers.

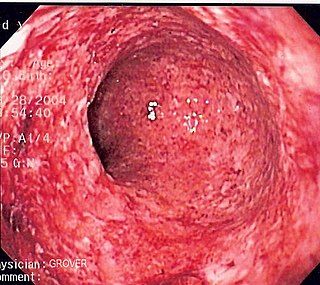
Ulcerative colitis (UC) is one of the two types of inflammatory bowel disease (IBD), with the other type being Crohn's disease. It is a long-term condition that results in inflammation and ulcers of the colon and rectum. The primary symptoms of active disease are abdominal pain and diarrhea mixed with blood (hematochezia). Weight loss, fever, and anemia may also occur. Often, symptoms come on slowly and can range from mild to severe. Symptoms typically occur intermittently with periods of no symptoms between flares. Complications may include abnormal dilation of the colon (megacolon), inflammation of the eye, joints, or liver, and colon cancer.

Enteritis is inflammation of the small intestine. It is most commonly caused by food or drink contaminated with pathogenic microbes, such as Serratia, but may have other causes such as NSAIDs, radiation therapy as well as autoimmune conditions like coeliac disease. Symptoms may include abdominal pain, cramping, diarrhoea, dehydration, and fever. Related diseases of the gastrointestinal (GI) system may involve inflammation of the stomach and large intestine.

Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, with Crohn's disease and ulcerative colitis (UC) being the principal types. Crohn's disease affects the small intestine and large intestine, as well as the mouth, esophagus, stomach and the anus, whereas UC primarily affects the colon and the rectum.

Diverticulosis is the condition of having multiple pouches (diverticula) in the colon that are not inflamed. These are outpockets of the colonic mucosa and submucosa through weaknesses of muscle layers in the colon wall. Diverticula do not cause symptoms in most people. Diverticular disease occurs when diverticula become clinically inflamed, a condition known as diverticulitis.

Colitis is swelling or inflammation of the large intestine (colon). Colitis may be acute and self-limited or long-term. It broadly fits into the category of digestive diseases.
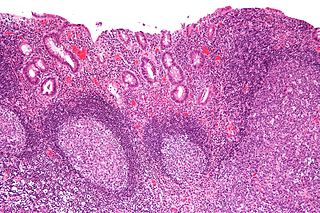
Diversion colitis is an inflammation of the colon which can occur as a complication of ileostomy or colostomy, where symptoms may occur between one month and three years following surgery. It also occurs frequently in a neovagina created by colovaginoplasty, with varying delay after the original procedure. Despite the presence of a variable degree of inflammation the most suggestive histological feature remains the prominent lymphoid aggregates.
Pouchitis is an umbrella term for inflammation of the ileal pouch, an artificial rectum surgically created out of ileum in patients who have undergone a proctocolectomy or total colectomy. The ileal pouch-anal anastomosis is created in the management of patients with ulcerative colitis, indeterminate colitis, familial adenomatous polyposis, cancer, or rarely, other colitides.

Microscopic colitis refers to two related medical conditions which cause diarrhea: collagenous colitis and lymphocytic colitis. Both conditions are characterized by the presence of chronic non-bloody watery diarrhea, normal appearances on colonoscopy and characteristic histopathology findings of inflammatory cells.

Lower gastrointestinal bleeding (LGIB) is any form of gastrointestinal bleeding in the lower gastrointestinal tract. LGIB is a common reason for seeking medical attention at a hospital's emergency department. LGIB accounts for 30–40% of all gastrointestinal bleeding and is less common than upper gastrointestinal bleeding (UGIB). It is estimated that UGIB accounts for 100–200 per 100,000 cases versus 20–27 per 100,000 cases for LGIB. Approximately 85% of lower gastrointestinal bleeding involves the large intestine, 10% are from bleeds that are actually upper gastrointestinal bleeds, and 3–5% involve the small intestine.
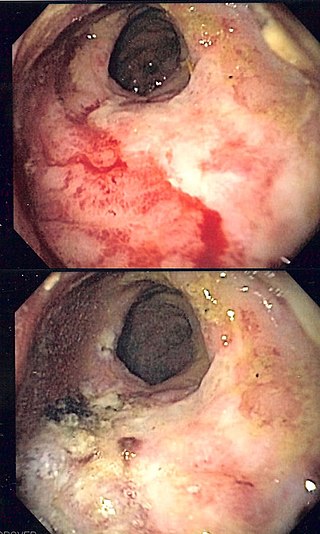
Radiation proctitis or radiation proctopathy is a condition characterized by damage to the rectum after exposure to x-rays or other ionizing radiation as a part of radiation therapy. Radiation proctopathy may occur as acute inflammation called "acute radiation proctitis" or with chronic changes characterized by radiation associated vascular ectasiae (RAVE) and chronic radiation proctopathy. Radiation proctitis most commonly occurs after pelvic radiation treatment for cancers such as cervical cancer, prostate cancer, bladder cancer, and rectal cancer. RAVE and chronic radiation proctopathy involves the lower intestine, primarily the sigmoid colon and the rectum, and was previously called chronic radiation proctitis, pelvic radiation disease and radiation enteropathy.

Collagenous colitis is an inflammatory condition of the colon. Together with the related condition lymphocytic colitis, it is a subtype of microscopic colitis, which is characterized by inflammation that specifically affects the colon, and a clinical presentation that involves watery diarrhea but a lack of rectal bleeding. Microscopic colitis does not usually cause macroscopic changes to the colon that allow a visual diagnosis during colonoscopy, instead causing microscopic changes that can be detected through histopathological examination of colonic biopsies. The nature of these microscopic changes is what differentiates collagenous from lymphocytic colitis, with the characteristic finding in collagenous colitis being depositions of collagen in the connective tissue between the colonic glands. Collagenous colitis, and microscopic colitis as a whole, is sometimes considered to be an inflammatory bowel disease (IBD) along with Crohn's disease and ulcerative colitis. However, little is known about the etiology of microscopic colitis, and so the degree of similarity to the inflammatory bowel diseases is uncertain.

Ischemic colitis is a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply (ischemia). Although uncommon in the general population, ischemic colitis occurs with greater frequency in the elderly, and is the most common form of bowel ischemia. Causes of the reduced blood flow can include changes in the systemic circulation or local factors such as constriction of blood vessels or a blood clot. In most cases, no specific cause can be identified.
Management of ulcerative colitis involves first treating the acute symptoms of the disease, then maintaining remission. Ulcerative colitis is a form of colitis, a disease of the intestine, specifically the large intestine or colon, that includes characteristic ulcers, or open sores, in the colon. The main symptom of active disease is usually diarrhea mixed with blood, of gradual onset which often leads to anaemia. Ulcerative colitis is, however, a systemic disease that affects many parts of the body outside the intestine.

Pancolitis or universal colitis, in its most general sense, refers to inflammation of the entire large intestine comprising the cecum, ascending, transverse, descending, sigmoid colon and rectum. It can be caused by a variety of things such as inflammatory bowel disease, more specifically a severe form of ulcerative colitis. A diagnosis can be made using a number of techniques but the most accurate method is direct visualization via a colonoscopy. Symptoms are similar to those of ulcerative colitis but more severe and affect the entire large intestine. Patients generally exhibit symptoms including rectal bleeding as a result of ulcers, pain in the abdominal region, inflammation in varying degrees, and diarrhea, fatigue, fever, and night sweats. Due to the loss of function in the large intestine patients may lose large amounts of weight from being unable to procure nutrients from food. In other cases the blood loss from ulcers can result in anemia which can be treated with iron supplements. Additionally, due to the chronic nature of most cases of pancolitis, patients have a higher chance of developing colorectal cancer.

Cytomegalovirus colitis is an inflammation of the colon.
Checkpoint inhibitor induced colitis is an inflammatory condition affecting the colon (colitis), which is caused by cancer immunotherapy. Symptoms typically consist of diarrhea, abdominal pain and rectal bleeding. Less commonly, nausea and vomiting may occur, which may suggest the present of gastroenteritis. The severity of diarrhea and colitis are graded based on the frequency of bowel movements and symptoms of colitis, respectively.

Segmental colitis associated with diverticulosis (SCAD) is a condition characterized by localized inflammation in the colon, which spares the rectum and is associated with multiple sac-like protrusions or pouches in the wall of the colon (diverticulosis). Unlike diverticulitis, SCAD involves inflammation of the colon between diverticula, while sparing the diverticular orifices. SCAD may lead to abdominal pain, especially in the left lower quadrant, intermittent rectal bleeding and chronic diarrhea.
A rectal stricture is a chronic and abnormal narrowing or constriction of the lumen of the rectum which presents a partial or complete obstruction to the movement of bowel contents. A rectal stricture is located deeper inside the body compared to an anal stricture. Sometimes other terms with wider meaning are used, such as anorectal stricture, colorectal stricture or rectosigmoid stricture.
References
- ↑ K. Harish, Severe colitis induced by soap enemas, Indian J. Gastroent., 2006 "Severe colitis induced by soap enemas K Harish, J Tony, R Sunilkumar, Thomas Varghese - Indian J Gastroenterol". Archived from the original on 2006-10-16. Retrieved 2006-07-23.
- 1 2 3 Sheibani, Sarah; Gerson, Lauren B. (February 2008). "Chemical Colitis". Journal of Clinical Gastroenterology. 42 (2): 115–121. doi:10.1097/MCG.0b013e318151470e. PMID 18209577.
- ↑ Ahishali, Emel; Uygur-Bayramiçli, Oya; Dolapçioğlu, Can; Dabak, Reşat; Mengi, Alperen; Işik, Aygün; Ermiş, Elvan (December 2009). "Chemical Colitis Due to Glutaraldehyde: Case Series and Review of the Literature". Digestive Diseases and Sciences. 54 (12): 2541–2545. doi:10.1007/s10620-008-0630-2. PMID 19104938.
- ↑ Ahn, Yura; Hong, Gil-Sun; Lee, Ju Hee; Lee, Choong Wook; Kim, Seon-Ok (7 November 2020). "Ischemic colitis after enema administration: Incidence, timing, and clinical features". World Journal of Gastroenterology. 26 (41): 6442–6454. doi: 10.3748/wjg.v26.i41.6442 . PMC 7656214 . PMID 33244204.
- ↑ Diarra, Brahima; Roudie, Jean; Ehua Somian, Francis; Coulibaly, Adama (June 2004). "Caustic burns of rectum and colon in emergencies". The American Journal of Surgery. 187 (6): 785–789. doi:10.1016/j.amjsurg.2003.10.019. PMID 15191876.