Related Research Articles
In neuroscience, an F wave is one of several motor responses which may follow the direct motor response (M) evoked by electrical stimulation of peripheral motor or mixed nerves. F-waves are the second of two late voltage changes observed after stimulation is applied to the skin surface above the distal region of a nerve, in addition to the H-reflex which is a muscle reaction in response to electrical stimulation of innervating sensory fibers. Traversal of F-waves along the entire length of peripheral nerves between the spinal cord and muscle, allows for assessment of motor nerve conduction between distal stimulation sites in the arm and leg, and related motoneurons (MN's) in the cervical and lumbosacral cord. F-waves are able to assess both afferent and efferent loops of the alpha motor neuron in its entirety. As such, various properties of F-wave motor nerve conduction are analyzed in nerve conduction studies (NCS), and often used to assess polyneuropathies, resulting from states of neuronal demyelination and loss of peripheral axonal integrity.
An evoked potential or evoked response is an electrical potential in a specific pattern recorded from a specific part of the nervous system, especially the brain, of a human or other animals following presentation of a stimulus such as a light flash or a pure tone. Different types of potentials result from stimuli of different modalities and types. Evoked potential is distinct from spontaneous potentials as detected by electroencephalography (EEG), electromyography (EMG), or other electrophysiologic recording method. Such potentials are useful for electrodiagnosis and monitoring that include detections of disease and drug-related sensory dysfunction and intraoperative monitoring of sensory pathway integrity.

In neuroanatomy, the trigeminal nerve (lit. triplet nerve), also known as the fifth cranial nerve, cranial nerve V, or simply CN V, is a cranial nerve responsible for sensation in the face and motor functions such as biting and chewing; it is the most complex of the cranial nerves. Its name (trigeminal, from Latin tri- 'three' and -geminus 'twin') derives from each of the two nerves (one on each side of the pons) having three major branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). The ophthalmic and maxillary nerves are purely sensory, whereas the mandibular nerve supplies motor as well as sensory (or "cutaneous") functions. Adding to the complexity of this nerve is that autonomic nerve fibers as well as special sensory fibers (taste) are contained within it.

A transcutaneous electrical nerve stimulation is a device that produces mild electric current to stimulate the nerves for therapeutic purposes. TENS, by definition, covers the complete range of transcutaneously applied currents used for nerve excitation, but the term is often used with a more restrictive intent, namely, to describe the kind of pulses produced by portable stimulators used to reduce pain. The unit is usually connected to the skin using two or more electrodes which are typically conductive gel pads. A typical battery-operated TENS unit is able to modulate pulse width, frequency, and intensity. Generally, TENS is applied at high frequency (>50 Hz) with an intensity below motor contraction or low frequency (<10 Hz) with an intensity that produces motor contraction. More recently, many TENS units use a mixed frequency mode which alleviates tolerance to repeated use. Intensity of stimulation should be strong but comfortable with greater intensities, regardless of frequency, producing the greatest analgesia. While the use of TENS has proved effective in clinical studies, there is controversy over which conditions the device should be used to treat.

Functional electrical stimulation (FES) is a technique that uses low-energy electrical pulses to artificially generate body movements in individuals who have been paralyzed due to injury to the central nervous system. More specifically, FES can be used to generate muscle contraction in otherwise paralyzed limbs to produce functions such as grasping, walking, bladder voiding and standing. This technology was originally used to develop neuroprostheses that were implemented to permanently substitute impaired functions in individuals with spinal cord injury (SCI), head injury, stroke and other neurological disorders. In other words, a person would use the device each time he or she wanted to generate a desired function. FES is sometimes also referred to as neuromuscular electrical stimulation (NMES).

Electromyography (EMG) is a technique for evaluating and recording the electrical activity produced by skeletal muscles. EMG is performed using an instrument called an electromyograph to produce a record called an electromyogram. An electromyograph detects the electric potential generated by muscle cells when these cells are electrically or neurologically activated. The signals can be analyzed to detect abnormalities, activation level, or recruitment order, or to analyze the biomechanics of human or animal movement. Needle EMG is an electrodiagnostic medicine technique commonly used by neurologists. Surface EMG is a non-medical procedure used to assess muscle activation by several professionals, including physiotherapists, kinesiologists and biomedical engineers. In computer science, EMG is also used as middleware in gesture recognition towards allowing the input of physical action to a computer as a form of human-computer interaction.
Electroneuronography or electroneurography (ENoG) is a neurological non-invasive test used to study the facial nerve in cases of muscle weakness in one side of the face. The technique of electroneuronography was first used by Esslen and Fisch in 1979 to describe a technique that examines the integrity and conductivity of peripheral nerves. In modern use, ENoG is used to describe study of the facial nerve, while the term nerve conduction study is employed for other nerves.

Electrotherapy is the use of electrical energy as a medical treatment. In medicine, the term electrotherapy can apply to a variety of treatments, including the use of electrical devices such as deep brain stimulators for neurological disease. The term has also been applied specifically to the use of electric current to speed up wound healing. The use of EMS is also very wide for dealing with muscular pain. Additionally, the term "electrotherapy" or "electromagnetic therapy" has also been applied to a range of alternative medical devices and treatments. Evidence supporting the effectiveness of electrotherapy is limited.

A nerve conduction study (NCS) is a medical diagnostic test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body. These tests may be performed by medical specialists such as clinical neurophysiologists, physical therapists, physiatrists, and neurologists who subspecialize in electrodiagnostic medicine. In the United States, neurologists and physiatrists receive training in electrodiagnostic medicine (performing needle electromyography as part of residency training and, in some cases, acquire additional expertise during a fellowship in clinical neurophysiology, electrodiagnostic medicine, or neuromuscular medicine. Outside the US, clinical neurophysiologists learn needle EMG and NCS testing.
Pulpitis is inflammation of dental pulp tissue. The pulp contains the blood vessels, the nerves, and connective tissue inside a tooth and provides the tooth's blood and nutrients. Pulpitis is mainly caused by bacterial infection which itself is a secondary development of caries. It manifests itself in the form of a toothache.

Rheobase is a measure of membrane potential excitability. In neuroscience, rheobase is the minimal current amplitude of infinite duration that results in the depolarization threshold of the cell membranes being reached, such as an action potential or the contraction of a muscle. In Greek, the root rhe translates to "current or flow", and basi means "bottom or foundation": thus the rheobase is the minimum current that will produce an action potential or muscle contraction.

Chronaxie is the minimum time required for an electric current double the strength of the rheobase to stimulate a muscle or a neuron. Rheobase is the lowest intensity with indefinite pulse duration which just stimulated muscles or nerves. Chronaxie is dependent on the density of voltage-gated sodium channels in the cell, which affect that cell's excitability. Chronaxie varies across different types of tissue: fast-twitch muscles have a lower chronaxie, slow-twitch muscles have a higher one. Chronaxie is the tissue-excitability parameter that permits choice of the optimum stimulus pulse duration for stimulation of any excitable tissue. Chronaxie (c) is the Lapicque descriptor of the stimulus pulse duration for a current of twice rheobasic (b) strength, which is the threshold current for an infinitely long-duration stimulus pulse. Lapicque showed that these two quantities (c,b) define the strength-duration curve for current: I = b(1+c/d), where d is the pulse duration. However, there are two other electrical parameters used to describe a stimulus: energy and charge. The minimum energy occurs with a pulse duration equal to chronaxie. Minimum charge (bc) occurs with an infinitely short-duration pulse. Choice of a pulse duration equal to 10c requires a current of only 10% above rheobase (b). Choice of a pulse duration of 0.1c requires a charge of 10% above the minimum charge (bc).
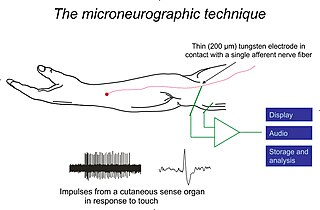
Microneurography is a neurophysiological method employed to visualize and record the traffic of nerve impulses that are conducted in peripheral nerves of waking human subjects. It can also be used in animal recordings. The method has been successfully employed to reveal functional properties of a number of neural systems, e.g. sensory systems related to touch, pain, and muscle sense as well as sympathetic activity controlling the constriction state of blood vessels. To study nerve impulses of an identified nerve, a fine tungsten needle microelectrode is inserted into the nerve and connected to a high input impedance differential amplifier. The exact position of the electrode tip within the nerve is then adjusted in minute steps until the electrode discriminates nerve impulses of interest. A unique feature and a significant strength of the microneurography method is that subjects are fully awake and able to cooperate in tests requiring mental attention, while impulses in a representative nerve fibre or set of nerve fibres are recorded, e.g. when cutaneous sense organs are stimulated or subjects perform voluntary precision movements.

Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A and B are myelinated. Group C fibers include postganglionic fibers in the autonomic nervous system (ANS), and nerve fibers at the dorsal roots. These fibers carry sensory information.
Repetitive nerve stimulation is a variant of the nerve conduction study where electrical stimulation is delivered to a motor nerve repeatedly several times per second. By observing the change in the muscle electrical response (CMAP) after several stimulations, a physician can assess for the presence of a neuromuscular junction disease, and differentiate between presynaptic and postsynaptic conditions. The test was first described by German neurologist Friedrich Jolly in 1895, and is also known as Jolly's test.
Electroanalgesia is a form of analgesia, or pain relief, that uses electricity to ease pain. Electrical devices can be internal or external, at the site of pain (local) or delocalized throughout the whole body. It works by interfering with the electric currents of pain signals, inhibiting them from reaching the brain and inducing a response; different from traditional analgesics, such as opiates which mimic natural endorphins and NSAIDs that help relieve inflammation and stop pain at the source. Electroanalgesia has a lower addictive potential and poses less health threats to the general public, but can cause serious health problems, even death, in people with other electrical devices such as pacemakers or internal hearing aids, or with heart problems.
A depolarizing prepulse (DPP) is an electrical stimulus that causes the potential difference measured across a neuronal membrane to become more positive or less negative, and precedes another electrical stimulus. DPPs may be of either the voltage or current stimulus variety and have been used to inhibit neural activity, selectively excite neurons, and increase the pain threshold associated with electrocutaneous stimulation.
Somatosensory evoked potential is the electrical activity of the brain that results from the stimulation of touch. SEP tests measure that activity and are a useful, noninvasive means of assessing somatosensory system functioning. By combining SEP recordings at different levels of the somatosensory pathways, it is possible to assess the transmission of the afferent volley from the periphery up to the cortex. SEP components include a series of positive and negative deflections that can be elicited by virtually any sensory stimuli. For example, SEPs can be obtained in response to a brief mechanical impact on the fingertip or to air puffs. However, SEPs are most commonly elicited by bipolar transcutaneous electrical stimulation applied on the skin over the trajectory of peripheral nerves of the upper limb or lower limb, and then recorded from the scalp. In general, somatosensory stimuli evoke early cortical components, generated in the contralateral primary somatosensory cortex (S1), related to the processing of the physical stimulus attributes. About 100 ms after stimulus application, additional cortical regions are activated, such as the secondary somatosensory cortex (S2), and the posterior parietal and frontal cortices, marked by a parietal P100 and bilateral frontal N140. SEPs are routinely used in neurology today to confirm and localize sensory abnormalities, to identify silent lesions and to monitor changes during surgical procedures.
Electromyoneurography (EMNG) is the combined use of electromyography and electroneurography This technique allows for the measurement of a peripheral nerve's conduction velocity upon stimulation (electroneurography) alongside electrical recording of muscular activity (electromyography). Their combined use proves to be clinically relevant by allowing for both the source and location of a particular neuromuscular disease to be known, and for more accurate diagnoses.
Neuromodulation is "the alteration of nerve activity through targeted delivery of a stimulus, such as electrical stimulation or chemical agents, to specific neurological sites in the body". It is carried out to normalize – or modulate – nervous tissue function. Neuromodulation is an evolving therapy that can involve a range of electromagnetic stimuli such as a magnetic field (rTMS), an electric current, or a drug instilled directly in the subdural space. Emerging applications involve targeted introduction of genes or gene regulators and light (optogenetics), and by 2014, these had been at minimum demonstrated in mammalian models, or first-in-human data had been acquired. The most clinical experience has been with electrical stimulation.
References
- ↑ Whatham, Andrew R (2013). "The value of clinical electrophysiology in the assessment of the eye and visual system in the era of advanced imaging". Clinical and Experimental Optometry. 97: 99–115. doi: 10.1111/cxo.12085 .
- 1 2 3 4 5 Andrew J. Robinson, Lynn Snyder-Mackler. "Clinical Electrophysiology: Electrotherapy and Electrophysiologic Testing," Lippincott Williams & Wilkins, 1994, ISBN 0-683-07817-8