Bacterial vaginosis (BV) is an infection of the vagina caused by excessive growth of bacteria. Common symptoms include increased vaginal discharge that often smells like fish. The discharge is usually white or gray in color. Burning with urination may occur. Itching is uncommon. Occasionally, there may be no symptoms. Having BV approximately doubles the risk of infection by a number of sexually transmitted infections, including HIV/AIDS. It also increases the risk of early delivery among pregnant women.
Nongonococcal urethritis (NGU) is inflammation of the urethra that is not caused by gonorrheal infection.
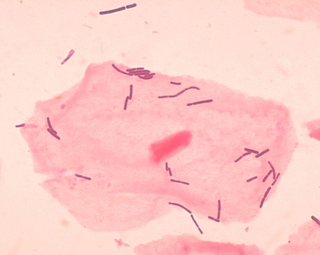
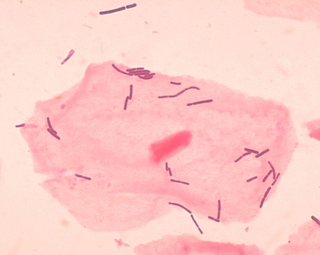
Gardnerella vaginalis is a species of Gram-variable-staining facultative anaerobic bacteria. The organisms are small non-spore-forming, nonmotile coccobacilli.
Vaginitis, also known as vulvovaginitis, is inflammation of the vagina and vulva. Symptoms may include itching, burning, pain, discharge, and a bad smell. Certain types of vaginitis may result in complications during pregnancy.
Mycoplasma hominis is a species of bacteria in the genus Mycoplasma. M. hominis has the ability to penetrate the interior of human cells. Along with ureaplasmas, mycoplasmas are the smallest free-living organisms known.

Ureaplasma urealyticum is a bacterium belonging to the genus Ureaplasma and the family Mycoplasmataceae in the order Mycoplasmatales. This family consists of the genera Mycoplasma and Ureaplasma. Its type strain is T960. There are two known biovars of this species; T960 and 27. These strains of bacteria are commonly found as commensals in the urogenital tracts of human beings, but overgrowth can lead to infections that cause the patient discomfort. Unlike most bacteria, Ureaplasma urealyticum lacks a cell wall making it unique in physiology and medical treatment.

Vaginal discharge is a mixture of liquid, cells, and bacteria that lubricate and protect the vagina. This mixture is constantly produced by the cells of the vagina and cervix, and it exits the body through the vaginal opening. The composition, amount, and quality of discharge varies between individuals and can vary throughout the menstrual cycle and throughout the stages of sexual and reproductive development. Normal vaginal discharge may have a thin, watery consistency or a thick, sticky consistency, and it may be clear or white in color. Normal vaginal discharge may be large in volume but typically does not have a strong odor, nor is it typically associated with itching or pain. While most discharge is considered physiologic or represents normal functioning of the body, some changes in discharge can reflect infection or other pathological processes. Infections that may cause changes in vaginal discharge include vaginal yeast infections, bacterial vaginosis, and sexually transmitted infections. The characteristics of abnormal vaginal discharge vary depending on the cause, but common features include a change in color, a foul odor, and associated symptoms such as itching, burning, pelvic pain, or pain during sexual intercourse.
Atopobium is a genus of Actinomycetota, in the family Coriobacteriaceae. Atopobium species are anaerobic, Gram-positive rod-shaped or elliptical bacteria found as single elements or in pairs or short chains.
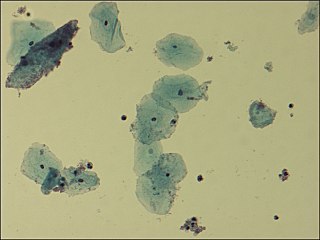
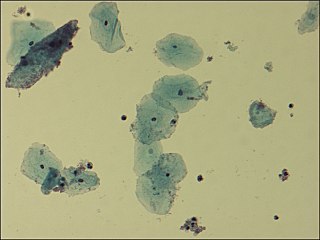
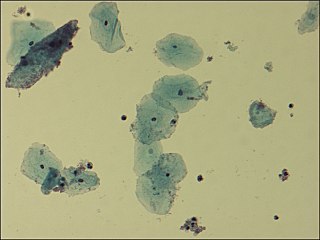
The Nugent Score is a Gram stain scoring system for vaginal swabs to diagnose bacterial vaginosis (BV). The Nugent score is calculated by assessing for the presence of large Gram-positive rods, small Gram-variable rods, and curved Gram-variable rods. A score of 7 to 10 is consistent with bacterial vaginosis without culture. The Nugent Score is now rarely used by physicians due to the time it takes to read the slides and requires the use of a trained microscopist. Bacterial vaginosis diagnosis is done by evaluating the pH, the presences of Lactobacillus spp. versus a mixed flora consisting of Gardnerella vaginalis, Bacteroides spp, Mobiluncus spp, and Mycoplasma hominis. The Amsel Criteria for bacterial vaginosis includes pH, evaluating the presence of clue cells, white discharge and an odor of amines after mixing with KOH.
Fusobacterium nucleatum is a Gram-negative, anaerobic oral bacterium, commensal to the human oral cavity, that plays a role in periodontal disease. This organism is commonly recovered from different monocultured microbial and mixed infections in humans and animals. In health and disease, it is a key component of periodontal plaque due to its abundance and its ability to coaggregate with other bacteria species in the oral cavity.
Vaginal flora, vaginal microbiota or vaginal microbiome are the microorganisms that colonize the vagina. They were discovered by the German gynecologist Albert Döderlein in 1892 and are part of the overall human flora. The amount and type of bacteria present have significant implications for an individual's overall health. The primary colonizing bacteria of a healthy individual are of the genus Lactobacillus, such as L. crispatus, and the lactic acid they produce is thought to protect against infection by pathogenic species.
Mobiluncus is a genus of Gram-positive, anaerobic, rod-shaped bacteria. These bacteria may be stained either Gram-negative or Gram-variable. However, they are classified as Gram-positive rods due to the fact that they possess a Gram-positive cell wall, lack endotoxin and are sensitive to vancomycin, erythromycin and ampicillin, but resistant to colistin.
Prevotella is a genus of Gram-negative bacteria.
Gardnerella is a genus of Gram-variable-staining facultative anaerobic bacteria.

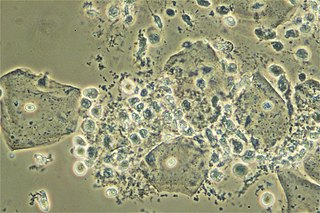
A vaginal wet mount is a gynecologic test wherein a sample of vaginal discharge is observed by wet mount microscopy by placing the specimen on a glass slide and mixing with a salt solution. It is used to find the cause of vaginitis and vulvitis.
The vaginal flora in pregnancy, or vaginal microbiota in pregnancy, is different from the vaginal flora before sexual maturity, during reproductive years, and after menopause. A description of the vaginal flora of pregnant women who are immunocompromised is not covered in this article. The composition of the vaginal flora significantly differs in pregnancy. Bacteria or viruses that are infectious most often have no symptoms.
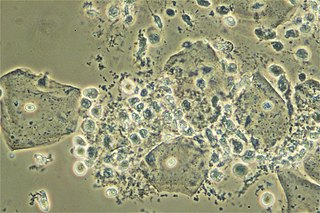
Aerobic vaginitis (AV) is a form of vaginitis first described by Donders et al. in 2002. It is characterized by a more or less severe disruption of the lactobacillary flora, along with inflammation, atrophy, and the presence of a predominantly aerobic microflora, composed of enteric commensals or pathogens.

The vaginal epithelium is the inner lining of the vagina consisting of multiple layers of (squamous) cells. The basal membrane provides the support for the first layer of the epithelium-the basal layer. The intermediate layers lie upon the basal layer, and the superficial layer is the outermost layer of the epithelium. Anatomists have described the epithelium as consisting of as many as 40 distinct layers of cells. The mucus found on the epithelium is secreted by the cervix and uterus. The rugae of the epithelium create an involuted surface and result in a large surface area that covers 360 cm2. This large surface area allows the trans-epithelial absorption of some medications via the vaginal route.

Lactobacillus vaccines are used in the therapy and prophylaxis of non-specific bacterial vaginitis and trichomoniasis. The vaccines consist of specific inactivated strains of Lactobacilli, called "aberrant" strains in the relevant literature dating from the 1980s. These strains were isolated from the vaginal secretions of patients with acute colpitis. The lactobacilli in question are polymorphic, often shortened or coccoid in shape and do not produce an acidic, anti-pathogenic vaginal environment. A colonization with aberrant lactobacilli has been associated with an increased susceptibility to vaginal infections and a high rate of relapse following antimicrobial treatment. Intramuscular administration of inactivated aberrant lactobacilli provokes a humoral immune response. The production of specific antibodies both in serum and in the vaginal secretion has been demonstrated. As a result of the immune stimulation, the abnormal lactobacilli are inhibited, the population of normal, rod-shaped lactobacilli can grow and exert its defense functions against pathogenic microorganisms.