Related Research Articles
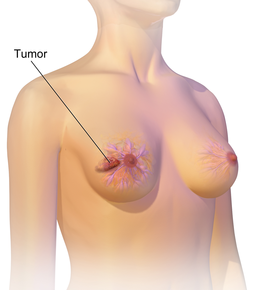
Breast cancer is cancer that develops from breast tissue. Signs of breast cancer may include a lump in the breast, a change in breast shape, dimpling of the skin, fluid coming from the nipple, a newly inverted nipple, or a red or scaly patch of skin. In those with distant spread of the disease, there may be bone pain, swollen lymph nodes, shortness of breath, or yellow skin.
Menarche is the first menstrual cycle, or first menstrual bleeding, in female humans. From both social and medical perspectives, it is often considered the central event of female puberty, as it signals the possibility of fertility.
Oophorectomy is the surgical removal of an ovary or ovaries. The surgery is also called ovariectomy, but this term is mostly used in reference to animals, e.g. the surgical removal of ovaries from laboratory animals. Removal of the ovaries of females is the biological equivalent of castration of males; the term castration is only occasionally used in the medical literature to refer to oophorectomy of women. In veterinary medicine, the removal of ovaries and uterus is called ovariohysterectomy (spaying) and is a form of sterilization.

Uterine cancer, also known as womb cancer, includes two types of cancer that develop from the tissues of the uterus. Endometrial cancer forms from the lining of the uterus, and uterine sarcoma forms from the muscles or support tissue of the uterus. Endometrial cancer accounts for approximately 90% of all uterine cancers in the United States. Symptoms of endometrial cancer include changes in vaginal bleeding or pain in the pelvis. Symptoms of uterine sarcoma include unusual vaginal bleeding or a mass in the vagina.

The Heart Protection Study was a randomized controlled trial run by the Clinical Trial Service Unit, and funded by the Medical Research Council (MRC) and the British Heart Foundation (BHF) in the United Kingdom. It studied the use of the cholesterol lowering drug, simvastatin 40 mg and vitamin supplementation in people who were at risk of cardiovascular disease. It was led by Jane Armitage, an epidemiologist at the Clinical Trial Service Unit.

The Women's Health Initiative (WHI) was a series of clinical studies initiated by the U.S. National Institutes of Health (NIH) in 1991, to address major health issues causing morbidity and mortality in postmenopausal women. It consisted of three clinical trials (CT) and an observational study (OS). In particular, randomized controlled trials were designed and funded that addressed cardiovascular disease, cancer, and osteoporosis.
The abortion–breast cancer hypothesis is a pseudoscientific belief that having an induced abortion can increase the risk of getting breast cancer. This hypothesis is at odds with mainstream scientific opinion and is rejected by major medical professional organizations. In early pregnancy, hormone levels increase, leading to breast growth. The hypothesis proposes that if this process is altered by an abortion, then more immature cells could be left behind, and that these immature cells could increase the risk of breast cancer over time.
Progestogen-only pills or progestin-only pills (POP) are contraceptive pills that contain only synthetic progestogens (progestins) and do not contain estrogen. They are colloquially known as mini pills.
The Nurses' Health Study is a series of prospective studies that examine epidemiology and the long-term effects of nutrition, hormones, environment, and nurses' work-life on health and disease development. The studies have been among the largest investigations into risk factors for major chronic diseases ever conducted. The Nurses' Health Studies have led to many insights on health and well-being, including cancer prevention, cardiovascular disease, and type 2 diabetes. They have included clinicians, epidemiologists, and statisticians at the Channing Laboratory, Harvard Medical School, Harvard School of Public Health, and several Harvard-affiliated hospitals, including Brigham and Women's Hospital, Dana–Farber Cancer Institute, Children's Hospital Boston, and Beth Israel Deaconess Medical Center.
Sarah C. Darby is Professor of Medical Statistics at the University of Oxford. Her research has focused the beneficial effects of smoking cessation, the risk of lung cancer from residential radon, and treatments for early breast cancer. She is also a Principal Scientist with the Cancer Research UK in the Clinical Trial Service Unit (CTSU) and Epidemiological Studies Unit at the Nuffield Department of Clinical Medicine, at the Radcliffe Infirmary, Oxford.
Risk factors for breast cancer may be divided into preventable and non-preventable. Their study belongs in the field of epidemiology. Breast cancer, like other forms of cancer, can result from multiple environmental and hereditary risk factors. The term "environmental", as used by cancer researchers, means any risk factor that is not genetically inherited.
Dame Valerie Beral AC DBE FRS FRCOG FMedSci is an Australian-born British epidemiologist, academic and a preeminent specialist in breast cancer epidemiology. She is Professor of Epidemiology, a Fellow of Green Templeton College, Oxford and has been the Head of the Cancer Epidemiology Unit at the University of Oxford and Cancer Research UK since 1989.
The Million Women Study is a study of women’s health analysing data from more than one million women aged 50 and over, led by Dame Valerie Beral and a team of researchers at the Cancer Epidemiology Unit, University of Oxford. It is a collaborative project between Cancer Research UK and the National Health Service (NHS), with additional funding from the Medical Research Council (UK).
Hormone replacement therapy (HRT), also known as menopausal hormone therapy or postmenopausal hormone therapy, is a form of hormone therapy used to treat symptoms associated with female menopause. These symptoms can include hot flashes, vaginal atrophy, accelerated skin aging, vaginal dryness, decreased muscle mass, sexual dysfunction, and bone loss. They are in large part related to the diminished levels of sex hormones that occur during menopause.

Myra Sally Hunter is Professor of Clinical Health Psychology at the Institute of Psychiatry, Psychology and Neuroscience, King's College, London, and a Clinical and Health Psychologist at the South London and Maudsley NHS Foundation Trust.
Kathleen I. Pritchard, is the head of oncology at Sunnybrook Health Sciences Centre in Toronto, Canada, specializing in breast cancer therapies, and leading the clinical trials division of the centre. She has authored numerous studies on women's health, breast cancer, hormone replacement therapy, public health, and research methodology. According to Thomson Reuters, Pritchard was one of the most cited researchers in the world in 2014 and 2015.
Estrogen deprivation therapy, also known as endocrine therapy, is a form of hormone therapy that is used in the treatment of breast cancer. Modalities include antiestrogens or estrogen blockers such as selective estrogen receptor modulators (SERMs) like tamoxifen, selective estrogen receptor degraders like fulvestrant, and aromatase inhibitors like anastrozole and ovariectomy.

The UK Coronavirus Cancer Monitoring Project or UKCCMP is a clinician-led reporting project established to safeguard, monitor and protect individuals living with cancer from COVID-19 across the United Kingdom.
The timing hypothesis, gap hypothesis, or critical window hypothesisfor menopausal hormone therapy is a scientific theory that the benefits and risks of menopausal hormone therapy vary depending on the amount of time a woman has been in menopause upon initiation of treatment. More specifically, it is thought that hormone therapy may be protective against coronary heart disease in women who initiate it in early menopause but may be harmful in women who start it in late menopause. The timing hypothesis may also extend to risks of breast cancer and Alzheimer's disease with hormone therapy. It is thought that the increase in breast cancer risk may be greater in women who start hormone therapy in early menopause but may be lower or that even decreased risk of breast cancer may occur in women who start in late menopause. The influence of hormone therapy on depressive symptoms may additionally be influenced by menopausal stage, with significant benefit seen in perimenopausal women but not in postmenopausal women. The timing hypothesis is potentially able to resolve conflicting findings between large observational studies and randomized controlled trials on long-term health outcomes with menopausal hormone therapy.
References
- 1 2 Collaborative Group on Hormonal Factors in Breast Cancer (September 2019). "Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence". Lancet. 394 (10204): 1159–1168. doi:10.1016/S0140-6736(19)31709-X. PMC 6891893 . PMID 31474332.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (June 1996). "Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53 297 women with breast cancer and 100 239 women without breast cancer from 54 epidemiological studies" (PDF). Lancet. 347 (9017): 1713–27. doi:10.1016/s0140-6736(96)90806-5. PMID 8656904. S2CID 36136756.
- ↑ "Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52 705 women with breast cancer and 108 411 women without breast cancer". The Lancet. 350 (9084): 1047–1059. 1997. doi:10.1016/S0140-6736(97)08233-0. ISSN 0140-6736. S2CID 54389746.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (2012). "Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies". The Lancet Oncology. 13 (11): 1141–1151. doi: 10.1016/S1470-2045(12)70425-4 . ISSN 1470-2045. PMC 3488186 . PMID 23084519.