In medicine, a prosthesis, or a prosthetic implant, is an artificial device that replaces a missing body part, which may be lost through physical trauma, disease, or a condition present at birth. Prostheses are intended to restore the normal functions of the missing body part. A person who has undergone an amputation is sometimes referred to as an amputee, however, this term may be offensive. Rehabilitation for someone with an amputation is primarily coordinated by a physiatrist as part of an inter-disciplinary team consisting of physiatrists, prosthetists, nurses, physical therapists, and occupational therapists. Prostheses can be created by hand or with computer-aided design (CAD), a software interface that helps creators design and analyze the creation with computer-generated 2-D and 3-D graphics as well as analysis and optimization tools.

A dental technician is a member of the dental team who, upon prescription from a dental clinician, constructs custom-made restorative and dental appliances.

A dental implant is a prosthesis that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, or facial prosthesis or to act as an orthodontic anchor. The basis for modern dental implants is a biological process called osseointegration, in which materials such as titanium or zirconia form an intimate bond to the bone. The implant fixture is first placed so that it is likely to osseointegrate, then a dental prosthetic is added. A variable amount of healing time is required for osseointegration before either the dental prosthetic is attached to the implant or an abutment is placed which will hold a dental prosthetic or crown.
Oral and maxillofacial surgery is a surgical specialty focusing on reconstructive surgery of the face, facial trauma surgery, the mouth, head and neck, and jaws, as well as facial plastic surgery including cleft lip and cleft palate surgery.
Osseointegration is the direct structural and functional connection between living bone and the surface of a load-bearing artificial implant. A more recent definition defines osseointegration as "functional ankylosis ", where new bone is laid down directly on the implant surface and the implant exhibits mechanical stability. Osseointegration has enhanced the science of medical bone and joint replacement techniques as well as dental implants and improving prosthetics for amputees.
Prosthodontics, also known as dental prosthetics or prosthetic dentistry, is the area of dentistry that focuses on dental prostheses. It is one of 12 dental specialties recognized by the American Dental Association (ADA), Royal College of Surgeons of England, Royal College of Surgeons of Edinburgh, Royal College of Surgeons of Ireland, Royal College of Surgeons of Glasgow, Royal College of Dentists of Canada, and Royal Australasian College of Dental Surgeons. The ADA defines it as "the dental specialty pertaining to the diagnosis, treatment planning, rehabilitation and maintenance of the oral function, comfort, appearance and health of patients with clinical conditions associated with missing or deficient teeth or oral and maxillofacial tissues using biocompatible substitutes."
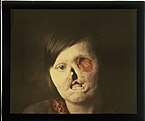
A facial prosthetic or facial prosthesis is an artificial device used to change or adapt the outward appearance of a person's face or head.

Hemifacial microsomia (HFM) is a congenital disorder that affects the development of the lower half of the face, most commonly the ears, the mouth and the mandible. It usually occurs on one side of the face, but both sides are sometimes affected. If severe, it may result in difficulties in breathing due to obstruction of the trachea—sometimes even requiring a tracheotomy. With an incidence in the range of 1:3500 to 1:4500, it is the second most common birth defect of the face, after cleft lip and cleft palate. HFM shares many similarities with Treacher Collins syndrome.

Enucleation is the removal of the eye that leaves the eye muscles and remaining orbital contents intact. This type of ocular surgery is indicated for a number of ocular tumors, in eyes that have sustained severe trauma, and in eyes that are otherwise blind and painful.
An ocularist specializes in the fabrication and fitting of ocular prostheses for people who have lost an eye or eyes due to trauma or illness. The fabrication process for a custom made eye typically includes taking an impression of the eye socket, shaping a plastic shell, painting the iris, and then fitting the ocular prostheses. Prefabricated ocular prostheses with different colored iris are also available. An ocularist may select the stock eye that is most closely matched to patient's iris color. However, due to better adaptation, comfort, and aesthetics, custom-made ocular prostheses are more accepted. In addition to creating the prosthetic eye, an ocularist shows the patient how to care for and handle the prosthesis.

A palatal lift prosthesis is a prosthesis that addresses a condition referred to as palatopharyngeal incompetence. Palatopharyngeal incompetence broadly refers to a muscular inability to sufficiently close the port between the nasopharynx and oropharynx during speech and/or swallowing. An inability to adequately close the palatopharyngeal port during speech results in hypernasalance that, depending upon its severity, can render speakers difficult to understand or unintelligible. The potential for compromised intelligibility secondary to hypernasalance is underscored when consideration is given to the fact that only three English language phonemes – /m/, /n/, and /ng/ – are pronounced with an open palatopharyngeal port. Furthermore, an impaired ability to effect a closure of the palatopharyngeal port while swallowing can result in the nasopharyngeal regurgitation of liquid or solid boluses.

A palatal obturator is a prosthesis that totally occludes an opening such as an oronasal fistula. They are similar to dental retainers, but without the front wire. Palatal obturators are typically short-term prosthetics used to close defects of the hard/soft palate that may affect speech production or cause nasal regurgitation during feeding. Following surgery, there may remain a residual orinasal opening on the palate, alveolar ridge, or vestibule of the larynx. A palatal obturator may be used to compensate for hypernasality and to aid in speech therapy targeting correction of compensatory articulation caused by the cleft palate. In simpler terms, a palatal obturator covers any fistulas in the roof of the mouth that lead to the nasal cavity, providing the wearer with a plastic/acrylic, removable roof of the mouth, which aids in speech, eating, and proper air flow.

Breast prostheses are breast forms intended to look like breasts. They are often used temporarily or permanently by women after mastectomy or lumpectomy procedures, but may also be used by for aesthetic purposes. There are a number of materials and designs; although, the most common construction is gel in a plastic film meant to feel similar to a person's skin. Prostheses may be purchased at a surgical supply store, pharmacy, custom lingerie shop, or even through private services that come to a person's home. There are many types of ready made breast prostheses including full or standard prostheses, partial prostheses such as shell prostheses, and stick on prostheses. Customized options are also available from specialty shops, which are moulded to fit an individual's chest by taking an impression of the breast(s). The areola and nipple may be replicated as part of the breast form or as separate nipple prosthesis. Both custom made and off-the shelf breast prostheses come in varieties that are designed to either be held in a pocket in a specially designed mastectomy bra or attached to the skin via adhesive or other methods and worn with a standard bra. There are many factors to consider when selecting breast prostheses such as different types and the care they require, insurance coverage, and psychosocial effects.

Anaplastology is a branch of medicine dealing with the prosthetic rehabilitation of an absent, disfigured or malformed anatomically critical location of the face or body. The term anaplastology was coined by Walter G. Spohn and is used worldwide.

An ocular prosthesis, artificial eye or glass eye is a type of craniofacial prosthesis that replaces an absent natural eye following an enucleation, evisceration, or orbital exenteration. The prosthesis fits over an orbital implant and under the eyelids. Though often referred to as a glass eye, the ocular prosthesis roughly takes the shape of a convex shell and is made of medical grade plastic acrylic. A few ocular prostheses today are made of cryolite glass. A variant of the ocular prosthesis is a very thin hard shell known as a scleral shell which can be worn over a damaged or eviscerated eye. Makers of ocular prosthetics are known as ocularists. An ocular prosthesis does not provide vision; this would be a visual prosthesis. Someone with an ocular prosthesis is altogether blind on the affected side and has monocular vision.

The Le Fortfractures are a pattern of midface fractures originally described by the French surgeon, René Le Fort, in the early 1900s. He described three distinct fracture patterns. Although not always applicable to modern-day facial fractures, the Le Fort type fracture classification is still utilized today by medical providers to aid in describing facial trauma for communication, documentation, and surgical planning. Several surgical techniques have been established for facial reconstruction following Le Fort fractures, including maxillomandibular fixation (MMF) and open reduction and internal fixation (ORIF). The main goal of any surgical intervention is to re-establish occlusion, or the alignment of upper and lower teeth, to ensure the patient is able to eat. Complications following Le Fort fractures rely on the anatomical structures affected by the inciding injury.

A nose prosthesis is a craniofacial prosthesis for someone who no longer has their original nose. Nose prostheses are designed by anaplastologists who have their patients referred to them by ear, nose, and throat doctors and plastic surgeons.

Nipple/Areola prostheses are made of silicone by breast prosthesis manufacturers and anaplastologists for breast cancer survivors who were treated for breast cancer with a mastectomy. Prostheses can be worn weeks after a mastectomy, breast reconstruction, or even nipple reconstruction. As an inexpensive and convenient alternative to surgery, patients may choose to wear them anytime during treatment. Patients who ultimately find nipple prostheses thought that they should be informed of them during the consultation prior to mastectomy.
Alveoloplasty is a surgical pre-prosthetic procedure performed to facilitate removal of teeth, and smoothen or reshape the jawbone for prosthetic and cosmetic purposes. In this procedure, the bony edges of the alveolar ridge and its surrounding structures is made smooth, redesigned or recontoured so that a well-fitting, comfortable, and esthetic prosthesis may be fabricated or implants may be surgically inserted. This pre-prosthetic surgery which may include bone grafting prepares the mouth to receive a prosthesis or implants by improving the condition and quality of the supporting structures so they can provide support, better retention and stability to the prosthesis.
Alloplasty is a surgical procedure performed to substitute and repair defects within the body with the use of synthetic material. It can also be performed in order to bridge wounds. The process of undergoing alloplasty involves the construction of an alloplastic graft through the use of computed tomography (CT), rapid prototyping and "the use of computer-assisted virtual model surgery." Each alloplastic graft is individually constructed and customised according to the patient's defect to address their personal health issue. Alloplasty can be applied in the form of reconstructive surgery. An example where alloplasty is applied in reconstructive surgery is in aiding cranial defects. The insertion and fixation of alloplastic implants can also be applied in cosmetic enhancement and augmentation. Since the inception of alloplasty, it has been proposed that it could be a viable alternative to other forms of transplants. The biocompatibility and customisation of alloplastic implants and grafts provides a method that may be suitable for both minor and major medical cases that may have more limitations in surgical approach. Although there has been evidence that alloplasty is a viable method for repairing and substituting defects, there are disadvantages including suitability of patient bone quality and quantity for long term implant stability, possibility of rejection of the alloplastic implant, injuring surrounding nerves, cost of procedure and long recovery times. Complications can also occur from inadequate engineering of alloplastic implants and grafts, and poor implant fixation to bone. These include infection, inflammatory reactions, the fracture of alloplastic implants and prostheses, loosening of implants or reduced or complete loss of osseointegration.