Sinus node dysfunction (SND), also known as sick sinus syndrome (SSS), is a group of abnormal heart rhythms (arrhythmias) usually caused by a malfunction of the sinus node, the heart's primary pacemaker. Tachycardia-bradycardia syndrome is a variant of sick sinus syndrome in which the arrhythmia alternates between fast and slow heart rates.

The sinoatrial node is a group of cells known as pacemaker cells, located in the wall of the right atrium of the heart. These cells have the ability to spontaneously produce an electrical impulse, that travels through the electrical conduction system of the heart causing it to contract. In a healthy heart, the SA node continuously produces action potentials, setting the rhythm of the heart, and so is known as the heart's natural pacemaker. The rate of action potentials produced is influenced by the nerves that supply it.

The atrioventricular node or AV node is a part of the electrical conduction system of the heart that coordinates the top of the heart. It electrically connects the atria and ventricles. The AV node lies at the lower back section of the interatrial septum near the opening of the coronary sinus, and conducts the normal electrical impulse from the atria to the ventricles. The AV node is quite compact.

Discovered in 1893 by Swiss-born cardiologist and anatomist Wilhelm His Jr., the bundle of His (BH) or His bundle (HB) ( "hiss") is a collection of heart muscle cells specialized for electrical conduction. As part of the electrical conduction system of the heart, it transmits the electrical impulses from the atrioventricular node to the point of the apex of the fascicular branches via the bundle branches. The fascicular branches then lead to the Purkinje fibers, which provide electrical conduction to the ventricles, causing the cardiac muscle of the ventricles to contract at a paced interval.

Third-degree atrioventricular block is a medical condition in which the nerve impulse generated in the sinoatrial node in the atrium of the heart can not propagate to the ventricles.
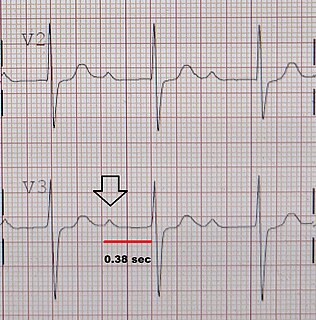
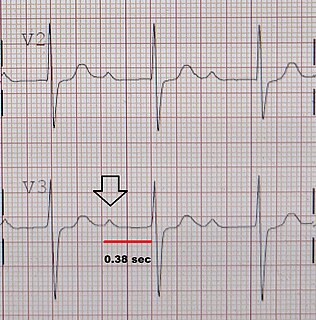
First-degree atrioventricular block is a disease of the electrical conduction system of the heart in which electrical impulses conduct from the cardiac atria to the ventricles through the atrioventricular node more slowly than normal. First degree AV block does not generally cause any symptoms, but may progress to more severe forms of heart block such as second- and third-degree atrioventricular block. It is diagnosed using an electrocardiogram, and is defined as a PR interval greater than 200 milliseconds. First degree AV block affects 0.65-1.1% of the population with 0.13 new cases per 1000 persons each year.

Second-degree atrioventricular block is a disease of the electrical conduction system of the heart. It is a conduction block between the atria and ventricles. The presence of second-degree AV block is diagnosed when one or more of the atrial impulses fail to conduct to the ventricles due to impaired conduction. It is classified as a block of the AV node and is categorized in between first-degree and third degree blocks.

Supraventricular tachycardia (SVT) is an umbrella term for fast heart rhythms arising from the upper part of the heart. This is in contrast to the other group of fast heart rhythms - ventricular tachycardia, which start within the lower chambers of the heart. There are four main types of SVT: atrial fibrillation, atrial flutter, paroxysmal supraventricular tachycardia (PSVT) and Wolff–Parkinson–White syndrome. The symptoms of SVT include palpitations, feeling of faintness, sweating, shortness of breath, and/or chest pain.

AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.
Premature atrial contractions (PACs), also known as atrial premature complexes (APC) or atrial premature beats (APB), are a common cardiac dysrhythmia characterized by premature heartbeats originating in the atria. While the sinoatrial node typically regulates the heartbeat during normal sinus rhythm, PACs occur when another region of the atria depolarizes before the sinoatrial node and thus triggers a premature heartbeat. The exact cause of PACs is unclear; while several predisposing conditions exist, PACs commonly occur in healthy young and elderly people. Elderly people that get PACs usually don't need any further attention besides follow ups due to unclear evidence. PACs are often completely asymptomatic and may be noted only with Holter monitoring, but occasionally they can be perceived as a skipped beat or a jolt in the chest. In most cases, no treatment other than reassurance is needed for PACs, although medications such as beta blockers can reduce the frequency of symptomatic PACs.
Lown–Ganong–Levine syndrome (LGL) is a pre-excitation syndrome of the heart. Those with LGL syndrome have episodes of abnormal heart racing with a short PR interval and normal QRS complexes seen on their electrocardiogram when in a normal sinus rhythm. LGL syndrome was originally thought to be due to an abnormal electrical connection between the atria and the ventricles, but is now thought to be due to accelerated conduction through the atrioventricular node in the majority of cases. The syndrome is named after Bernard Lown, William Francis Ganong, Jr., and Samuel A. Levine.

In the heart's conduction system, Bachmann's bundle is a branch of the anterior internodal tract that resides on the inner wall of the left atrium. It is a broad band of cardiac muscle that passes from the right atrium, between the superior vena cava and the ascending aorta. Bachmann's bundle is, during normal sinus rhythm, the preferential path for electrical activation of the left atrium. It is therefore considered to be part of the "atrial conduction system" of the heart.

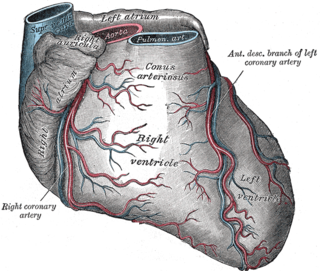
The sinoatrial nodal artery is an artery of the heart which supplies the sinoatrial node, the natural pacemaker center of the heart, and arises from the right coronary artery in around 60% of people. In about 40% of cases, the sinoatrial artery is a branch of the left circumflex coronary artery. In less than 1% of humans, the artery has an anomalous origin directly from the coronary sinus, descending aorta, or distal right coronary artery.
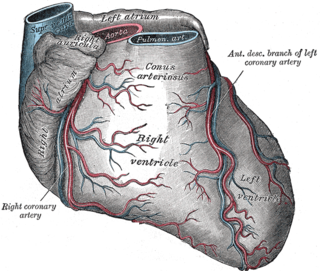
The atrioventricular nodal branch is a coronary artery that feeds the atrioventricular node, necessary for the excitation of the ventricles.

Primary tumors of the heart are extremely rare tumors that arise from the normal tissues that make up the heart. This is in contrast to secondary tumors of the heart, which are typically either metastatic from another part of the body, or infiltrate the heart via direct extension from the surrounding tissues.
The term dromotropic derives from the Greek word δρόμος drómos, meaning "running", a course, a race. A dromotropic agent is one which affects the conduction speed in the AV node, and subsequently the rate of electrical impulses in the heart.

Junctional tachycardia is a form of supraventricular tachycardia characterized by involvement of the AV node. It can be contrasted to atrial tachycardia. It is a tachycardia associated with the generation of impulses in a focus in the region of the atrioventricular node due to an A-V disassociation. In general, the AV junction's intrinsic rate is 40-60 bpm so an accelerated junctional rhythm is from 60-100bpm and then becomes junctional tachycardia at a rate of >100 bpm.
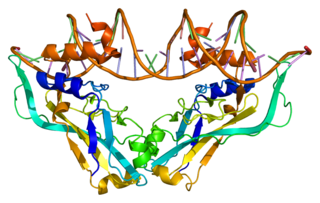
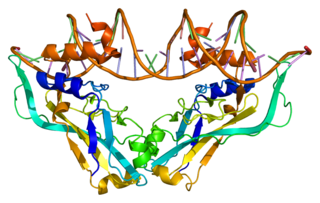
T-box transcription factor 2 Tbx2 is a transcription factor that is encoded by the Tbx2 gene on chromosome 17q21-22 in humans. This gene is a member of a phylogenetically conserved family of genes that share a common DNA-binding domain, the T-box. Tbx2 and Tbx3 are the only T-box transcription factors that act as transcriptional repressors rather than transcriptional activators, and are closely related in terms of development and tumorigenesis. This gene plays a significant role in embryonic and fetal development through control of gene expression, and also has implications in various cancers. Tbx2 is associated with numerous signaling pathways, BMP, TGFβ, Wnt, and FGF, which allow for patterning and proliferation during organogenesis in fetal development.

Junctional ectopic tachycardia (JET) is a rare syndrome of the heart that manifests in patients recovering from heart surgery. It is characterized by cardiac arrhythmia, or irregular beating of the heart, caused by abnormal conduction from or through the atrioventricular node. In newborns and infants up to 6 weeks old, the disease may also be referred to as His bundle tachycardia or congenital JET.

Arrhythmias, also known as cardiac arrhythmias,heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath or chest pain. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.