Related Research Articles

Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid agonist used for chronic pain and also for opioid dependence. It is used to treat chronic pain, and it is also used to treat addiction to heroin or other opioids. Prescribed for daily use, the medicine relieves cravings and removes withdrawal symptoms. Detoxification using methadone can be accomplished in less than a month, or it may be done gradually over as long as for the rest of the patient’s life. While a single dose has a rapid effect, maximum effect can take up to five days of use. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.
Drug rehabilitation is the process of medical or psychotherapeutic treatment for dependency on psychoactive substances such as alcohol, prescription drugs, and street drugs such as cannabis, cocaine, heroin or amphetamines. The general intent is to enable the patient to confront substance dependence, if present, and stop substance misuse to avoid the psychological, legal, financial, social, and physical consequences that can be caused.

Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids. Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are important components of OUD.

Buprenorphine is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider. In the United States, the combination formulation of buprenorphine/naloxone (Suboxone) is usually prescribed to discourage misuse by injection. Maximum pain relief is generally within an hour with effects up to 24 hours. Buprenorphine affects different types of opioid receptors in different ways. Depending on the type of receptor, it may be an agonist, partial agonist, or antagonist. In the treatment of opioid use disorder buprenorphine is an agonist/antagonist, meaning that it relieves withdrawal symptoms from other opioids and induces some euphoria, but also blocks the ability for many other opioids, including heroin, to cause an effect. Unlike full agonists like heroin or methadone, buprenorphine has a ceiling effect, such that taking more medicine will not increase the effects of the drug.

Naltrexone, sold under the brand names Revia and Vivitrol among others, is a medication primarily used to manage alcohol use or opioid use disorder by reducing cravings and feelings of euphoria associated with substance use disorder. It has also been found effective in the treatment of other addictions and may be used for them off-label. An opioid-dependent person should not receive naltrexone before detoxification. It is taken by mouth or by injection into a muscle. Effects begin within 30 minutes,though a decreased desire for opioids may take a few weeks to occur.
A methadone clinic, or substance use disorder services clinic (SUDS), is a clinic which has been established for the dispensing of medications used in the treatment of opiate dependence —historically and most commonly methadone, although buprenorphine is also increasingly prescribed. Medically assisted drug therapy treatment is indicated in patients who are opioid-dependent or have a history of opioid dependence. Methadone is a schedule II (USA) opioid analgesic, that is also prescribed for pain management. It is a long-acting opioid that can delay the opioid withdrawal symptoms that patients experience from taking short-acting opioids, like heroin, and allow time for detoxification. In the United States, by law, patients must receive methadone under the supervision of a physician, and dispensed through an opioid treatment program certified by the Substance Abuse and Mental Health Services Administration and registered with the Drug Enforcement Administration.
An opioid antagonist, or opioid receptor antagonist, is a receptor antagonist that acts on one or more of the opioid receptors.
Low-dose naltrexone (LDN) describes the off-label, experimental use of the medication naltrexone at low doses for diseases such as Crohn's disease and multiple sclerosis, but evidence for recommending such use is lacking.
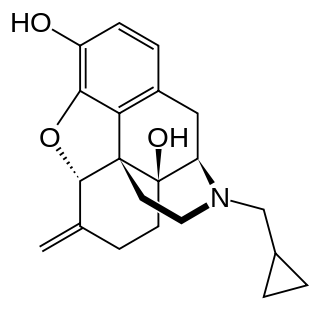
Nalmefene is an opioid antagonist medication used in the management of opioid overdose and alcohol dependence. It is taken by mouth or by injection.
The Drug Addiction Treatment Act of 2000, Title XXXV, Section 3502 of the Children's Health Act, permits physicians who meet certain qualifications to treat opioid addiction with Schedule III, IV, and V narcotic medications that have been specifically approved by the Food and Drug Administration for that indication.
Treatment Improvement Protocols (TIPs) are a series of best-practice manuals for the treatment of substance use and other related disorders. The TIP series is published by the Substance Abuse and Mental Health Services Administration (SAMHSA), an operational division of the U.S. Department of Health and Human Services.

Substance abuse prevention, also known as drug abuse prevention, is a process that attempts to prevent the onset of substance use or limit the development of problems associated with using psychoactive substances. Prevention efforts may focus on the individual or their surroundings. A concept that is known as "environmental prevention" focuses on changing community conditions or policies so that the availability of substances is reduced as well as the demand. Individual Substance Abuse Prevention, also known as drug abuse prevention involves numerous different sessions depending on the individual to help cease or reduce the use of substances. The time period to help a specific individual can vary based upon many aspects of an individual. The type of Prevention efforts should be based upon the individual's necessities which can also vary. Substance use prevention efforts typically focus on minors and young adults – especially between 12–35 years of age. Substances typically targeted by preventive efforts include alcohol, tobacco, marijuana, inhalants, coke, methamphetamine, steroids, club drugs, and opioids. Community advocacy against substance use is imperative due to the significant increase in opioid overdoses in the United States alone. It has been estimated that about one hundred and thirty individuals continue to lose their lives daily due to opioid overdoses alone.
Drug detoxification is variously the intervention in a case of physical dependence to a drug; the process and experience of a withdrawal syndrome; and any of various treatments for acute drug overdose.

An opioid overdose is toxicity due to excessive consumption of opioids, such as morphine, codeine, heroin, fentanyl, tramadol, and methadone. This preventable pathology can be fatal if it leads to respiratory depression, a lethal condition that can cause hypoxia from slow and shallow breathing. Other symptoms include small pupils, and unconsciousness, however its onset can depend on the method of ingestion, the dosage and individual risk factors. Although there were over 110,000 deaths in 2017 due to opioids, individuals who survived also faced adverse complications, including permanent brain damage.

Substance use disorder (SUD) is the persistent use of drugs despite substantial harm and adverse consequences as a result of their use. The National Institute of Mental Health (NIMH) states that “Substance use disorder (SUD) is a treatable mental disorder that affects a person's brain and behavior, leading to their inability to control their use of substances like legal or illegal drugs, alcohol, or medications. Symptoms can be moderate to severe, with addiction being the most severe form of SUD”. Substance use disorders (SUD) are considered to be a serious mental illness that fluctuates with the age that symptoms first start appearing in an individual, the time during which it exists and the type of substance that is used. It is not uncommon that those who have SUD also have other mental health disorders. Substance use disorders are characterized by an array of mental/emotional, physical, and behavioral problems such as chronic guilt; an inability to reduce or stop consuming the substance(s) despite repeated attempts; operating vehicles while intoxicated; and physiological withdrawal symptoms. Drug classes that are commonly involved in SUD include: alcohol, caffeine, cannabis, hallucinogens, inhalants, opioids, sedatives, hypnotics or anxiolytics, stimulants, tobacco

Charles P. O'Brien is a research scientist, medical educator and a leading expert in the science and treatment of addiction. He is board certified in neurology, psychiatry and addiction psychiatry. He is currently the Kenneth E. Appel Professor of Psychiatry, and vice chair of psychiatry, in the Perelman School of Medicine at the University of Pennsylvania.

In the United States, the opioid epidemic is an extensive ongoing overuse of opioid medications, both from medical prescriptions and illegal sources. The epidemic began in the United States in the late 1990s, according to the Centers for Disease Control and Prevention (CDC), when opioids were increasingly prescribed for pain management, resulting in a rise in overall opioid use throughout subsequent years. The great majority of Americans who use prescription opioids do not believe that they are misusing them.
JourneyPure is an American health care private organization that treats people experiencing substance use disorders and operates a network of treatment centers throughout the United States. The organization is notable for development of opioid and addiction treatment rehabilitation programs during the ongoing Opioid epidemic in the United States.
Kelly J. Clark is an American physician and psychiatrist known for her work in the fields of substance use disorder, addiction medicine, and addiction psychiatry.

Prescription drug addiction is the chronic, repeated use of a prescription drug in ways other than prescribed for, including using someone else’s prescription. A prescription drug is a pharmaceutical drug that may not be dispensed without a legal medical prescription. Drugs in this category are supervised due to their potential for misuse and Substance use disorder. The classes of medications most commonly abused are opioids, central nervous system (CNS) depressants and central nervous stimulants. In particular, prescription opioid is most commonly abused in the form of prescription analgesics.
References
- 1 2 "Pennsylvania opts for a different tool to assess drug abuse | Reading Eagle - NEWS". Reading Eagle. Retrieved September 12, 2017.
- ↑ Stateline, Pew's (April 27, 2016). "This Opioid Treatment Model That Provides All Levels Of Care Is Spawning Imitators". Huffington Post. Retrieved September 12, 2017.
- ↑ "Third of Philadelphians used prescription opioids in the last year, survey finds". Philly.com. Retrieved September 12, 2017.
- ↑ Freyer, Felice (December 20, 2015). "Drug may give those leaving jail a better shot at recovery". The Boston Globe. Retrieved September 11, 2017.
- ↑ "David R. Gastfriend M.D. : Executive Profile & Biography - Bloomberg". www.bloomberg.com. Retrieved September 11, 2017.
- ↑ "Treatment Research Institute names new CEO". www.bizjournals.com. August 14, 2014. Retrieved September 11, 2017.
- ↑ BioCorRx Inc. (September 12, 2017). "BioCorRx Announces Beta Launch of Mobile Application for Opioid and Alcohol Substance Use Disorder". Nasdaq Marketwired. Retrieved September 12, 2017.
- ↑ "BioCorRx Reports 12% Increase in Revenue and Provides Business Update for the Second Quarter of 2017". UPTICK Newswire. August 15, 2017. Retrieved September 11, 2017.
- 1 2 "Treatment Research Institute Approved for $13 Million Research Funding Award by the U.S. Patient-Centered Outcomes Research Institute". PRWeb. Retrieved September 11, 2017.
- 1 2 "General health clinics, specialty care will go head-to-head in opioid treatment study | Addiction Professional Magazine". www.addictionpro.com. Retrieved September 11, 2017.
- 1 2 3 "ASAM's Assessment Software CONTINUUM™ to be Used in Significant Clinical Trial". Continuum | ASAM Criteria Decision Engine. May 1, 2017. Retrieved September 12, 2017.
- 1 2 3 "A Simple Large Trial of Patient-Centered Care for Opioid Use Disorders in Federally Qualified Healthcare Centers and Specialty Care Settings". www.pcori.org. March 15, 2017. Retrieved September 12, 2017.
- ↑ "ASAM Patient Placement Criteria - Oversight and Revision" (PDF). May 2011. Retrieved September 11, 2017.
- ↑ Kolsky, Gretchen D. (November 1, 2006). "Current State AOD Agency Practices Regarding the Use of Patient Placement Criteria (PPC) - An Update" (PDF). www.asam.org. The National Association of State Alcohol and Drug Abuse Directors.
- ↑ Gamboa, Cesar (April 3, 2017). "Pennsylvania to adopt ASAM guidelines for addiction treatment • Addiction Now | Substance Abuse, Drug Addiction and Recovery News Source". Addiction Now | Substance Abuse, Drug Addiction and Recovery News Source. Retrieved September 12, 2017.
- ↑ "ASAM Criteria evolves into electronic tool | Behavioral Healthcare Magazine". www.behavioral.net. Retrieved September 12, 2017.
- ↑ "The Last Shot — ProPublica". ProPublica. Alec MacGillis. June 27, 2017. Retrieved September 11, 2017.
{{cite web}}: CS1 maint: others (link) - ↑ Krupitsky, Evgeny; Nunes, Edward V.; Ling, Walter; Illeperuma, Ari; Gastfriend, David R.; Silverman, Bernard L. (April 28, 2011). "Injectable extended-release naltrexone for opioid dependence: a double-blind, placebo-controlled, multicentre randomised trial" (PDF). The Lancet. 377 (9776): 1506–13. doi:10.1016/s0140-6736(11)60358-9. PMID 21529928. S2CID 16690413 . Retrieved June 11, 2017.
- ↑ "A Shot in the Dark: Can Vivitrol Help Us Control Our Addictions?". May 7, 2013.
- ↑ "ASAM Award Programs". www.asam.org. Retrieved September 11, 2017.
- ↑ "Faculty". Addiction eXecutives Industry Summit. Retrieved September 12, 2017.
- ↑ Center for Public Health Initiatives. "Evidence-based Public Health Week: From the Streets to the ER: The Opioid Analgesic Epidemic" (PDF). www.cphi.upenn.edu/. Retrieved September 12, 2017.
- ↑ "Profile: BioCorRx Inc". Reuters. Retrieved September 11, 2017.
- ↑ "Bloomberg: Company Overview of BioCorRx Inc". www.bloomberg.com. Retrieved September 11, 2017.