Related Research Articles

In physiology, an action potential (AP) occurs when the membrane potential of a specific cell location rapidly rises and falls: this depolarization then causes adjacent locations to similarly depolarize. Action potentials occur in several types of animal cells, called excitable cells, which include neurons, muscle cells, endocrine cells and in some plant cells.

The contraction of cardiac muscle in all animals is initiated by electrical impulses known as action potentials. The rate at which these impulses fire, controls the rate of cardiac contraction, that is, the heart rate. The cells that create these rhythmic impulses, setting the pace for blood pumping, are called pacemaker cells, and they directly control the heart rate. They make up the cardiac pacemaker, that is, the natural pacemaker of the heart. In most humans, the concentration of pacemaker cells in the sinoatrial (SA) node is the natural pacemaker, and the resultant rhythm is a sinus rhythm.
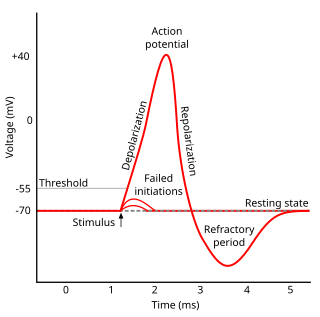
Refractoriness is the fundamental property of any object of autowave nature not to respond on stimuli, if the object stays in the specific refractory state. In common sense, refractory period is the characteristic recovery time, a period that is associated with the motion of the image point on the left branch of the isocline .

In electrocardiography, the ventricular cardiomyocyte membrane potential is about −90 mV at rest, which is close to the potassium reversal potential. When an action potential is generated, the membrane potential rises above this level in four distinct phases.
Hyperpolarization is a change in a cell's membrane potential that makes it more negative. It is the opposite of a depolarization. It inhibits action potentials by increasing the stimulus required to move the membrane potential to the action potential threshold.

The sinoatrial node is a group of cells located in the wall of the right atrium of the heart. These cells have the ability to spontaneously produce an electrical impulse, that travels through the heart via the electrical conduction system causing it to contract. In a healthy heart, the SA node continuously produces action potential, setting the rhythm of the heart and so is known as the heart's natural pacemaker. The rate of action potential production is influenced by nerves that supply it.
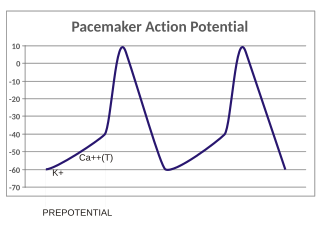
In the pacemaking cells of the heart (e.g., the sinoatrial node), the pacemaker potential (also called the pacemaker current) is the slow, positive increase in voltage across the cell's membrane (the membrane potential) that occurs between the end of one action potential and the beginning of the next action potential. This increase in membrane potential is what causes the cell membrane, which typically maintains a resting membrane potential of -70 mV, to reach the threshold potential and consequently fire the next action potential; thus, the pacemaker potential is what drives the self-generated rhythmic firing (automaticity) of pacemaker cells, and the rate of change (i.e., the slope) of the pacemaker potential is what determines the timing of the next action potential and thus the intrinsic firing rate of the cell. In a healthy sinoatrial node (SAN, a complex tissue within the right atrium containing pacemaker cells that normally determine the intrinsic firing rate for the entire heart), the pacemaker potential is the main determinant of the heart rate. Because the pacemaker potential represents the non-contracting time between heart beats (diastole), it is also called the diastolic depolarization. The amount of net inward current required to move the cell membrane potential during the pacemaker phase is extremely small, in the order of few pAs, but this net flux arises from time to time changing contribution of several currents that flow with different voltage and time dependence. Evidence in support of the active presence of K+, Ca2+, Na+ channels and Na+/K+ exchanger during the pacemaker phase have been variously reported in the literature, but several indications point to the “funny”(If) current as one of the most important.(see funny current). There is now substantial evidence that also sarcoplasmic reticulum (SR) Ca2+-transients participate to the generation of the diastolic depolarization via a process involving the Na–Ca exchanger.

The electrical conduction system of the heart transmits signals generated usually by the sinoatrial node to cause contraction of the heart muscle. The pacemaking signal generated in the sinoatrial node travels through the right atrium to the atrioventricular node, along the Bundle of His and through bundle branches to cause contraction of the heart muscle. This signal stimulates contraction first of the right and left atrium, and then the right and left ventricles. This process allows blood to be pumped throughout the body.
The cardiac action potential is a brief change in voltage across the cell membrane of heart cells. This is caused by the movement of charged atoms between the inside and outside of the cell, through proteins called ion channels. The cardiac action potential differs from action potentials found in other types of electrically excitable cells, such as nerves. Action potentials also vary within the heart; this is due to the presence of different ion channels in different cells.

In neuroscience, repolarization refers to the change in membrane potential that returns it to a negative value just after the depolarization phase of an action potential which has changed the membrane potential to a positive value. The repolarization phase usually returns the membrane potential back to the resting membrane potential. The efflux of potassium (K+) ions results in the falling phase of an action potential. The ions pass through the selectivity filter of the K+ channel pore.
Azimilide is a class ΙΙΙ antiarrhythmic drug. The agents from this heterogeneous group have an effect on the repolarization, they prolong the duration of the action potential and the refractory period. Also they slow down the spontaneous discharge frequency of automatic pacemakers by depressing the slope of diastolic depolarization. They shift the threshold towards zero or hyperpolarize the membrane potential. Although each agent has its own properties and will have thus a different function.
Cardioplegia is intentional and temporary cessation of cardiac activity, primarily for cardiac surgery.
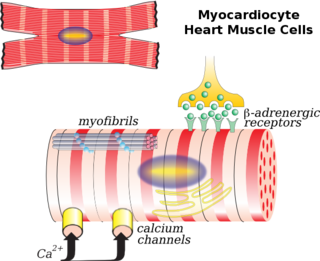
Cardiac muscle cells or cardiomyocytes are the muscle cells (myocytes) that make up the cardiac muscle. Each myocardial cell contains myofibrils, which are specialized organelles consisting of long chains of sarcomeres, the fundamental contractile units of muscle cells.
The pacemaker current is an electric current in the heart that flows through the HCN channel or pacemaker channel. Such channels are important parts of the electrical conduction system of the heart and form a component of the natural pacemaker.
The myogenic mechanism is how arteries and arterioles react to an increase or decrease of blood pressure to keep the blood flow constant within the blood vessel. Myogenic response refers to a contraction initiated by the myocyte itself instead of an outside occurrence or stimulus such as nerve innervation. Most often observed in smaller resistance arteries, this 'basal' tone may be useful in the regulation of organ blood flow and peripheral resistance, as it positions a vessel in a preconstricted state that allows other factors to induce additional constriction or dilation to increase or decrease blood flow.
Afterdepolarizations are abnormal depolarizations of cardiac myocytes that interrupt phase 2, phase 3, or phase 4 of the cardiac action potential in the electrical conduction system of the heart. Afterdepolarizations may lead to cardiac arrhythmias.
Cellular neuroscience is a branch of neuroscience concerned with the study of neurons at a cellular level. This includes morphology and physiological properties of single neurons. Several techniques such as intracellular recording, patch-clamp, and voltage-clamp technique, pharmacology, confocal imaging, molecular biology, two photon laser scanning microscopy and Ca2+ imaging have been used to study activity at the cellular level. Cellular neuroscience examines the various types of neurons, the functions of different neurons, the influence of neurons upon each other, and how neurons work together.
Cardiac physiology or heart function is the study of healthy, unimpaired function of the heart: involving blood flow; myocardium structure; the electrical conduction system of the heart; the cardiac cycle and cardiac output and how these interact and depend on one another.
N-(p-Amylcinnamoyl)anthranilic acid (ACA) is a modulator of various ion channels in the heart. ACA is an effective reversible inhibitor of calcium-activated chloride channels and, to a lesser extent, cAMP-activated chloride channels, without affecting L-type calcium channels. Calcium-activated chloride channels are believed to be involved in developing arrhythmia.

Budiodarone (ATI-2042) is an antiarrhythmic agent and chemical analog of amiodarone that is currently being studied in clinical trials. Amiodarone is considered the most effective antiarrhythmic drug available, but its adverse side effects, including hepatic, pulmonary and thyroid toxicity as well as multiple drug interactions, are discouraging its use. Budiodarone only differs in structure from amiodarone through the presence of a sec-butyl acetate side chain at position 2 of the benzofuran moiety. This side chain allows for budiodarone to have a shorter half-life in the body than amiodarone which allows it to have a faster onset of action and metabolism while still maintaining similar electrophysiological activity. The faster metabolism of budiodarone allows for fewer adverse side effects than amiodarone principally due to decreased levels of toxicity in the body.
References
- ↑ DiFrancesco D. (2006). Funny channels in the control of cardiac rhythm and mode of action of selective blockers. Pharmacol Res. 2006 May; 53(5):399-406.
- ↑ Bucchi A, Baruscotti M, Robinson RB, DiFrancesco D. (2007) Modulation of rate by autonomic agonists in SAN cells involves changes in diastolic depolarization and the pacemaker current. J Mol Cell Cardiol. Jul;43(1):39-48.