Psychosis is a condition of the mind or psyche that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.

Psychopharmacology is the scientific study of the effects drugs have on mood, sensation, thinking, behavior, judgment and evaluation, and memory. It is distinguished from neuropsychopharmacology, which emphasizes the correlation between drug-induced changes in the functioning of cells in the nervous system and changes in consciousness and behavior.

Chlorpromazine (CPZ), marketed under the brand names Thorazine and Largactil among others, is an antipsychotic medication. It is primarily used to treat psychotic disorders such as schizophrenia. Other uses include the treatment of bipolar disorder, severe behavioral problems in children including those with attention deficit hyperactivity disorder, nausea and vomiting, anxiety before surgery, and hiccups that do not improve following other measures. It can be given orally, by intramuscular injection, or intravenously.

The atypical antipsychotics (AAP), also known as second generation antipsychotics (SGAs) and serotonin–dopamine antagonists (SDAs), are a group of antipsychotic drugs largely introduced after the 1970s and used to treat psychiatric conditions. Some atypical antipsychotics have received regulatory approval for schizophrenia, bipolar disorder, irritability in autism, and as an adjunct in major depressive disorder.
Hormone therapy or hormonal therapy is the use of hormones in medical treatment. Treatment with hormone antagonists may also be referred to as hormonal therapy or antihormone therapy. The most general classes of hormone therapy are oncologic hormone therapy, hormone replacement therapy, androgen replacement therapy (ART), oral contraceptive pills, and Gender-affirming hormone therapy.

Hyperprolactinaemia is a condition characterized by abnormally high levels of prolactin in the blood. In women, normal prolactin levels average to about 13 ng/mL, while in men, they average 5 ng/mL. The upper normal limit of serum prolactin is typically between 15 to 25 ng/mL for both genders. Levels exceeding this range indicate hyperprolactinemia.
The dopamine hypothesis of schizophrenia or the dopamine hypothesis of psychosis is a model that attributes the positive symptoms of schizophrenia to a disturbed and hyperactive dopaminergic signal transduction. The model draws evidence from the observation that a large number of antipsychotics have dopamine-receptor antagonistic effects. The theory, however, does not posit dopamine overabundance as a complete explanation for schizophrenia. Rather, the overactivation of D2 receptors, specifically, is one effect of the global chemical synaptic dysregulation observed in this disorder.

Raloxifene, sold under the brand name Evista among others, is a medication used to prevent and treat osteoporosis in postmenopausal women and those on glucocorticoids. For osteoporosis it is less preferred than bisphosphonates. It is also used to reduce the risk of breast cancer in those at high risk. It is taken by mouth.
Latent inhibition (LI) is a technical term in classical conditioning, where a familiar stimulus takes longer to acquire meaning than a new stimulus. The term originated with Lubow and Moore in 1973. The LI effect is latent in that it is not exhibited in the stimulus pre-exposure phase, but rather in the subsequent test phase. "Inhibition", here, simply connotes that the effect is expressed in terms of relatively poor learning. The LI effect is extremely robust, appearing in both invertebrate and mammalian species that have been tested and across many different learning paradigms, thereby suggesting some adaptive advantages, such as protecting the organism from associating irrelevant stimuli with other, more important, events.
Sex and drugs refers to the influence of substances on sexual function and experience. Sex and drugs date back to ancient humans and have been interlocked throughout human history. Sexual performance is known as the execution of the act of sex and the quality of sexual activity. This includes elements such as libido, sexual function, sensation . Drugs are termed as any chemical substance that produces a physiological and or psychological change in an organism. Drugs categorized as psychoactive drugs, antihypertensive drugs, antihistamines, cancer treatment, and hormone medication have a significant impact on sexual performance. Various drugs result in different effects, both positive and negative. Negative effects may include low libido, erection issues, vaginal dryness and anorgasmia. Positive effects usually address these issues, overall enhancing sexual performance and contributing to a more enjoyable sexual experience. It is crucial to know that the impact of drugs on sexual performance varies among individuals, especially among different genders.

Coumestrol is a natural organic compound in the class of phytochemicals known as coumestans. Coumestrol was first identified as a compound with estrogenic properties by E. M. Bickoff in ladino clover and alfalfa in 1957. It has garnered research interest because of its estrogenic activity and prevalence in some foods, including soybeans, brussels sprouts, spinach and a variety of legumes. The highest concentrations of coumestrol are found in clover, Kala Chana, and Alfalfa sprouts.

Clinical neurochemistry is the field of neurological biochemistry which relates biochemical phenomena to clinical symptomatic manifestations in humans. While neurochemistry is mostly associated with the effects of neurotransmitters and similarly functioning chemicals on neurons themselves, clinical neurochemistry relates these phenomena to system-wide symptoms. Clinical neurochemistry is related to neurogenesis, neuromodulation, neuroplasticity, neuroendocrinology, and neuroimmunology in the context of associating neurological findings at both lower and higher level organismal functions.
The causes of schizophrenia that underlie the development of schizophrenia, a psychiatric disorder, are complex and not clearly understood. A number of hypotheses including the dopamine hypothesis, and the glutamate hypothesis have been put forward in an attempt to explain the link between altered brain function and the symptoms and development of schizophrenia.

Research into the mental disorder of schizophrenia, involves multiple animal models as a tool, including in the preclinical stage of drug development.
The epigenetics of schizophrenia is the study of how inherited epigenetic changes are regulated and modified by the environment and external factors and how these changes influence the onset and development of, and vulnerability to, schizophrenia. Epigenetics concerns the heritability of those changes, too. Schizophrenia is a debilitating and often misunderstood disorder that affects up to 1% of the world's population. Although schizophrenia is a heavily studied disorder, it has remained largely impervious to scientific understanding; epigenetics offers a new avenue for research, understanding, and treatment.
Sex differences in schizophrenia are widely reported. Men and women exhibit different rates of incidence and prevalence, age at onset, symptom expression, course of illness, and response to treatment. Reviews of the literature suggest that understanding the implications of sex differences on schizophrenia may help inform individualized treatment and positively affect outcomes.
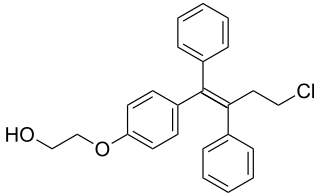
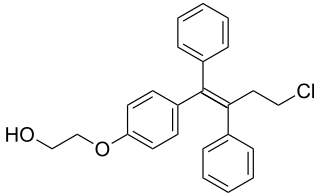
Ospemifene is an oral medication indicated for the treatment of dyspareunia – pain during sexual intercourse – encountered by some women, more often in those who are post-menopausal. Ospemifene is a selective estrogen receptor modulator (SERM) acting similarly to an estrogen on the vaginal epithelium, building vaginal wall thickness which in turn reduces the pain associated with dyspareunia. Dyspareunia is most commonly caused by "vulvar and vaginal atrophy."
Dopamine therapy is the regulation of levels of the neurotransmitter dopamine through the use of either agonists, or antagonists; and has been used in the treatment of disorders characterized by a dopamine imbalance. Dopamine replacement therapy (DRT) is an effective treatment for patients with decreased levels of dopamine. Often dopamine antagonists, compounds that activate dopamine receptors in the absence of that receptor's physiological ligand, the neurotransmitter dopamine, are used in this therapy. DRT has been shown to reduce symptoms and increase lifespan for patients with Parkinson's disease. Dopamine regulation plays a critical role in human mental and physical health. The neurons that contain the neurotransmitter are clustered in the midbrain region in an area called the substantia nigra. In Parkinson's patients, the death of dopamine-transmitting neurons in this area leads to abnormal nerve-firing patterns that cause motor problems. Research in patients with schizophrenia indicates abnormalities in dopamine receptor structure and function.
Dopamine supersensitivity psychosis is a hypothesis that attempts to explain the phenomenon in which psychosis occurs despite treatment with escalating doses of antipsychotics. Dopamine supersensitivity may be caused by the dopamine receptor D2 antagonizing effect of antipsychotics, causing a compensatory increase in D2 receptors within the brain that sensitizes neurons to endogenous release of the neurotransmitter dopamine. Because psychosis is thought to be mediated—at least in part—by the activity of dopamine at D2 receptors, the activity of dopamine in the presence of supersensitivity may paradoxically give rise to worsening psychotic symptoms despite antipsychotic treatment at a given dose. This phenomenon may co-occur with tardive dyskinesia, a rare movement disorder that may also be due to dopamine supersensitivity.
Immuno-psychiatry, according to Pariante, is a discipline that studies the connection between the brain and the immune system. It differs from psychoneuroimmunology by postulating that behaviors and emotions are governed by peripheral immune mechanisms. Depression, for instance, is seen as malfunctioning of the immune system.