Transfusion medicine is the branch of medicine that encompasses all aspects of the transfusion of blood and blood components including aspects related to hemovigilance. It includes issues of blood donation, immunohematology and other laboratory testing for transfusion-transmitted diseases, management and monitoring of clinical transfusion practices, patient blood management, therapeutic apheresis, stem cell collections, cellular therapy, and coagulation. Laboratory management and understanding of state and federal regulations related to blood products are also a large part of the field.
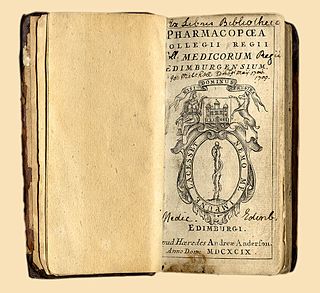
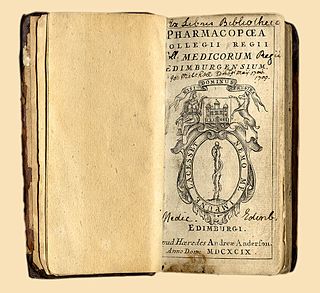
A pharmacopoeia, pharmacopeia, or pharmacopoea, in its modern technical sense, is a book containing directions for the identification of compound medicines, and published by the authority of a government or a medical or pharmaceutical society.

Good manufacturing practices (GMP) are the practices required in order to conform to the guidelines recommended by agencies that control the authorization and licensing of the manufacture and sale of food and beverages, cosmetics, pharmaceutical products, dietary supplements, and medical devices. These guidelines provide minimum requirements that a manufacturer must meet to assure that their products are consistently high in quality, from batch to batch, for their intended use. The rules that govern each industry may differ significantly; however, the main purpose of GMP is always to prevent harm from occurring to the end user. Additional tenets include ensuring the end product is free from contamination, that it is consistent in its manufacture, that its manufacture has been well documented, that personnel are well trained, and that the product has been checked for quality more than just at the end phase. GMP is typically ensured through the effective use of a quality management system (QMS).
A British Approved Name (BAN) is the official, non-proprietary, or generic name given to a pharmaceutical substance, as defined in the British Pharmacopoeia (BP).
The BAN is also the official name used in some countries across the world, because starting in 1953, proposed new names were evaluated by a panel of experts from WHO in conjunction with the BP commission to ensure naming consistency worldwide. There is also a British Approved Name (Modified) (BANM).

The regulation of therapeutic goods, defined as drugs and therapeutic devices, varies by jurisdiction. In some countries, such as the United States, they are regulated at the national level by a single agency. In other jurisdictions they are regulated at the state level, or at both state and national levels by various bodies, as in Australia.

The European Medicines Agency (EMA) is an agency of the European Union (EU) in charge of the evaluation and supervision of medicinal products. Prior to 2004, it was known as the European Agency for the Evaluation of Medicinal Products or European Medicines Evaluation Agency (EMEA).

The Medicines and Healthcare products Regulatory Agency (MHRA) is an executive agency of the Department of Health and Social Care in the United Kingdom which is responsible for ensuring that medicines and medical devices work and are acceptably safe.
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) is an initiative that brings together regulatory authorities and pharmaceutical industry to discuss scientific and technical aspects of pharmaceutical product development and registration.
The British Pharmacopoeia (BP) is the national pharmacopoeia of the United Kingdom. It is an annually published collection of quality standards for UK medicinal substances. It is used by individuals and organisations involved in pharmaceutical research, development, manufacture and testing.
In the experimental (non-clinical) research arena, good laboratory practice or GLP is a quality system of management controls for research laboratories and organizations to ensure the uniformity, consistency, reliability, reproducibility, quality, and integrity of products in development for human or animal health through non-clinical safety tests; from physio-chemical properties through acute to chronic toxicity tests.
NHS Blood and Transplant is an executive non-departmental public body of the United Kingdom's Department of Health and Social Care. It was established on 1 October 2005 to take over the responsibilities of two separate NHS agencies: UK Transplant, founded by Dr. Geoffrey Tovey in 1972, and the National Blood Service. Its remit is to provide a reliable, efficient supply of blood, organs and associated services to the NHS. Since NHSBT was established, the organisation has maintained or improved the quality of the services delivered to patients, stabilised the rising cost of blood, and centralised a number of corporate services.

The European Pharmacopoeia is a major regional pharmacopoeia which provides common quality standards throughout the pharmaceutical industry in Europe to control the quality of medicines, and the substances used to manufacture them. It is a published collection of monographs which describe both the individual and general quality standards for ingredients, dosage forms, and methods of analysis for medicines. These standards apply to medicines for both human and veterinary use.
The International Pharmacopoeia is a pharmacopoeia issued by the World Health Organization as a recommendation, with the aim to provide international quality specifications for pharmaceutical substances and dosage forms, together with supporting general methods of analysis, for global use. Its texts can be used or adapted by any WHO member state wishing to establish legal pharmaceutical requirements.
ISBT 128 is a global standard for the identification, labeling, and information transfer of medical products of human origin across international borders and disparate health care systems.

The Health Sciences Authority is a statutory board under the Ministry of Health of the Singapore Government, next to Outram Park MRT station.
The following outline is provided as an overview of and topical guide to clinical research:
The National Institute for Biological Standards and Control (NIBSC) is a government agency that works in the field of biological standardisation. It is part of the UK Medicines and Healthcare products Regulatory Agency (MHRA). It is responsible for developing and producing over 90% of the biological international standards in use around the world.
The Committee on Herbal Medicinal Products (HMPC), is the European Medicines Agency's committee responsible for elaborating the agency's opinions on herbal medicines.
An Official Medicines Control Laboratory (OMCL) is an official laboratory for the investigation and independent quality control of medicinal products and other similarly regulated substances.
The Spanish Agency of Medicines and Medical Devices (AEMPS) is a regulatory agency of the Government of Spain that acts as the highest sanitary authority in terms of medical safety on medicines, health products, cosmetics and personal care products.