Related Research Articles

Ophthalmology is a surgical subspecialty within medicine that deals with the diagnosis and treatment of eye disorders. A former term is oculism.

Cataract surgery, which is also called lens replacement surgery, is the removal of the natural lens of the human eye that has developed a cataract, an opaque or cloudy area. The eye's natural lens is usually replaced with an artificial intraocular lens (IOL).

Sankara Nethralaya is a not-for-profit missionary institution for ophthalmic care headquartered in Chennai, India. In the name "Sankara Nethralaya", "Sankara" is a reference to Lord Shiva and "Nethralaya" means "The Temple of the Eye". Sankara Nethralaya receives patients from India and abroad. Sankara Nethralaya has over 1000 employees and serves around 1500 patients per day, performing over 100 surgeries per day. The annual revenue as per the taxes is close to US$100 million.

Minto Ophthalmic Hospital is a government run specialty hospital in Bangalore treating diseases of the eye. Minto Ophthalmic Hospital,, was established in 1896, making it one of the oldest speciality eye hospitals in the world. The Hospital was started in Chikkapete area in 1896, moved to Lalbagh lodge in 1897 and later shifted to the present building in 1913 which was constructed during the reign of Nalwadi Krishnaraja Wadiyar IV, the King of Mysuru state. It is affiliated to the Bangalore Medical College and Research Institute, and is an institution of national importance.

Govindappa Venkataswamy, popularly known as Dr V., was an Indian ophthalmologist who dedicated his life to eliminate needless blindness. He was the founder and former chairman of Aravind Eye Hospitals. He is best known for developing a high quality, high volume, low-cost service delivery model that has restored sight to millions of people. Since inception, Aravind Eye Care System has seen over 55 million patients, and performed over 6.8 million surgeries. Over 50% of the organisation's patients pay either nothing or highly subsidised rates. Its scale and self-sustainability prompted a 1993 Harvard Business Case Study on the Aravind model.
Suseela Prabhakaran is an Indian ophthalmologist and chief ophthalmic surgeon at Divya Prabha Eye Hospital in Trivandrum, India. She started her career as a lecturer in ophthalmology in the Department of Medical Education at the state government of Kerala.
Sarojini Devi Eye Hospital is a Regional Institute of Ophthalmology and Government Ophthalmic hospital, a medical institution in Hyderabad, Telangana, India. It is named after Sarojini Naidu, a child prodigy, Indian independence activist and poet. It is affiliated to Osmania Medical College and Gandhi Medical College and serves as a teaching hospital. Originally, it included an ENT section, but it was separated and moved to separate premises in Hyderabad. Located very near to Mehdipatnam, it is situated near the starting point of the P.V. Narasimha Rao Expressway.

Lifeline Express is a charitable organization that attempts to reduce blindness in China. Since 1997, the organization has operated rainbow-coloured hospital "Eye-Trains," which provide free cataract surgery to patients in rural parts of China. In addition, Lifeline Express promotes ophthalmological training for Chinese doctors, through constructing training centers and inviting foreign doctors to China as consultants, and builds solar hot water systems in remote parts of China.
Sankurathri Foundation (SF) was established in 1989 by Dr. Chandra Sekhar Sankurathri in memory of his wife Manjari, son Kiran and daughter Sarada, who died in the bombing of Air India Flight 182 off the coast of Ireland on 23 June 1985.

Sanduk Ruit is an ophthalmologist from Nepal who has restored the sight of over 180,000 people across Africa and Asia using small-incision cataract surgery.

The eye care system in Ghana can be said to be one in its infant or growing stages. Today there are less than 300 eye care professionals taking care of the eye needs of over 23 million Ghanaians.
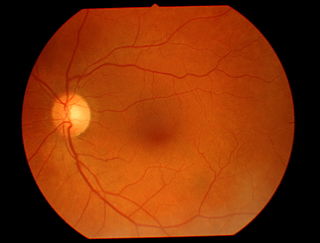
Teleophthalmology is a branch of telemedicine that delivers eye care through digital medical equipment and telecommunications technology. Today, applications of teleophthalmology encompass access to eye specialists for patients in remote areas, ophthalmic disease screening, diagnosis and monitoring; as well as distant learning.

The Organisation for the Prevention of Blindness is an international non-governmental organisation whose actions today focus exclusively on French-speaking countries in Africa. Their mission is to preserve and restore sight amongst some of the most under-privileged communities in the region. The OPC's principal actions concern blindness prevention, treatment and the elimination of blinding diseases, such as onchocerciasis, trachoma, glaucoma and cataracts as well as formal ophthalmological training.
Tilganga Institute of Ophthalmology, formerly called the Tilganga Eye Centre, in Nepal is the implementing body of the Nepal Eye Program, a non-profit, community based, non-government organization launched in 1992. It was founded in part by renowned ophthalmologist and cataract surgeon Sanduk Ruit. The current facility was opened in 1994. The World Health Organization recognized Tilganga Institute of Ophthalmology as a WHO Collaboration Centre of Ophthalmology in 2019. In Nepal, it is the second institute, and first institute in the field of ophthalmology to receive this designation. It provides various sub speciality services of Ophthalmology such as Cornea, Cataract & IOL, Glaucoma, Oculoplastic, Lacrimal and Ocular Oncology services, Pediatric Ophthalmology and Strabismus services, Vitreo-Retina, Uvea, Neuro ophthalmology and Optometry services.
The Himalayan Cataract Project (HCP) was created in 1994 by Dr. Geoffrey Tabin and Dr. Sanduk Ruit with a goal of establishing a sustainable eye care infrastructure in the Himalaya. HCP empowers local doctors to provide ophthalmic care through skills-transfer and education. From its beginning, HCP responds to a pressing need for eye care in the Himalayan region. With programs in Nepal, Ethiopia, Ghana, Bhutan and India they have been able to restore sight to over one million people since year since 1994.
Keiki R. Mehta, an Indian ophthalmologist, medical researcher and writer, is considered by many as the father of Phacoemulsification in India. He is the Chief Surgical and Medical Director at Mehta International Eye Institute, a Mumbai-based specialty eye hospital founded by him. He is known to be the first surgeon to perform a Radial keratotomy in India and is credited with the development of the first soft eye implant in the world, and the Keiki Mehta BP Valve Glaucoma Shunt, a medical implant used in the treatment of neovascular‚ congenital and uveitic glaucoma. He is a recipient of several honours including the Grand Honors Award of the National Eye Research Foundation, Chicago and the Triple Ribbon Award of the American Society for Cataract and Refractive Surgery. The Government of India awarded him the fourth highest civilian honour of the Padma Shri, in 2008, for his contributions to Medicine.

Community ophthalmology was described as a new discipline in medicine promoting eye health and blindness prevention through programs utilizing methodologies of public health, community medicine and ophthalmology in 1978. This new discipline was first proposed by Dr. Patricia E. Bath in 1978 after observations of epidemics rates of preventable blindness among under-served populations in urban areas in the US as well as under-served populations in so called third-world countries.
Anil Kumar Mandal is an Indian ophthalmologist and a consultant at L. V. Prasad Eye Institute, Hyderabad. Known for his research on glaucoma, Mandal is an elected fellow of the National Academy of Medical Sciences. The Council of Scientific and Industrial Research, the apex agency of the Government of India for scientific research, awarded him the Shanti Swarup Bhatnagar Prize for Science and Technology, one of the highest Indian science awards, for his contributions to Medical Sciences in 2003.
The Myanmar Eye Care Project (MECP) is focused on improving the delivery of critical eye care services to at-risk populations in Myanmar. Founded in 2002 and staffed entirely by ophthalmologists, it aims to end blindness in Myanmar. Myanmar is one of the poorest countries in Southeast Asia and has the highest rate of blindness in the world. Working with partners and a network of providers, MECP operates clinics that provide routine eye care, acute treatment, and surgeries to Myanmar's poor rural populations. MECP also builds eye care infrastructure in rural communities, trains indigenous physicians and nursing staff, and provides equipment.
Akshay Nair is an Indian ophthalmologist based in Mumbai, India. He specializes in oculoplastics, orbital surgery and ocular oncology. Currently, Dr. Nair is the Director of Ophthalmic plastic surgery and ocular oncology services at the Mumbai units of Dr. Agarwal's Eye Hospital: Advanced Eye Hospital and Institute and Aditya Jyot Eye Hospital.
References
- ↑ Kovai, Vilas; Krishnaiah, Sannapaneni; Shamanna, Bindiganavale Ramaswamy; Thomas, Ravi; Rao, Gullapalli N (2007). "Barriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh, South India". Indian Journal of Ophthalmology. 55 (5): 365–371. doi: 10.4103/0301-4738.33823 . ISSN 0301-4738. PMC 2636013 . PMID 17699946.
- ↑ "How India became a leader in low-cost, high-quality eye care". Devex. 31 October 2018. Retrieved 6 December 2018.