Fee splitting is the practice of sharing fees with professional colleagues, such as physicians or lawyers, in return for being sent referrals. [1]
This is essentially the payment of a commission to the referrer with the express intention of ensuring that the referring doctor directs referrals of patients to the payee.
In most parts of the world, the practice is considered unethical and unacceptable, hence fee splitting is often covert. The reason it is believed not to be in the interests of patients is because it represents a conflict of interest which may adversely affect patient care and well-being, since patients will not necessarily be referred to the most appropriate doctor to provide their on-going care but will instead be referred to those doctors or hospitals with whom the referring doctor has a "fee splitting" or commission payment type of arrangement. It is also called as 'CUT' (also spoken as Cee-You-Tee) practice in many parts of the world including India for its reference to a 'cut' from the patients bill.
Many countries do not allow promotion of health services via mass media, advertisements and other direct promotions, and in a significant way, information on pricing and quality of care institutions and medicines reaches to patient through their primary care physician, many of whom indulge in a referral fee split unethical practice to refer a patient for business to a higher specialist, brand prescription and admissions.
The situation in the US is not entirely clear. [2]
According to the World Medical Association, [3]
The AMA Code provides that payment by or to a physician solely for the referral of a patient is unethical as is the acceptance by a physician of payment of any kind, and in any form, from any source such as a pharmaceutical company or pharmacist or a manufacturer of medical appliances and devices, for referring a patient to that source. Another section specifies that clinics, laboratories, hospitals or other health care facilities which compensate physicians for referral of patients are engaged in fee-splitting, which is unethical.
Among its Definitions of Unprofessional Conduct, the "West Hudson Psychiatric Society Virtual Newsletter" (1997) lists "Offering, giving or receiving a fee for the referral of a patient (fee splitting), or permitting any person other than an employee or associate to share in your fee, who has not provided an appropriate service directly under your supervision." [4]
However, the practice, or something resembling it, tends to be tolerated – in Medicine, Money, and Morals: Physicians' Conflicts of Interest by Marc A. Rodwin, forms of fee splitting and commission paying for referrals remain common in the US and are in effect tolerated by key overseeing bodies such as the American Medical Association and Joint Commission International, or JCI. [5]
According to their website, the Joint Commission (JCI) have no published view on the issue of fee splitting, and in fact the Joint Commission stopped trying to provide guidance on medical ethics to American hospitals many years ago, preferring to concentrate on less challenging areas of healthcare assessment, despite the vast importance of medical ethics to patient safety. It is not clear if JCI operate to a similar level of standards when working outside of the US.
The popular group marketing website Groupon and other daily deal businesses have received the green light from some U.S. state bar associations, most notably North Carolina's State Bar formal opinion. [6] However, approved in some jurisdictions, Alabama and other state bar associations have chosen to dissent [7] from the NC state bar ruling, and have formally ruled in opposition to allowing daily deal websites as an ethical form of group marketing. Some state bar associations have yet to formally choose an opinion.
Fee splitting and similar practices are considered unequivocally unacceptable for the medical profession in the United Kingdom.
The practice is considered unethical, and offenders can be disciplined and even "struck off the medical register" (that is, lose their license to practice medicine). [8]
Fee splitting in the medical profession of various sorts has been alleged in Malta, [9] Singapore, [10] Thailand, [11] and India. [12]
In France, both dichotomie [13] (the sharing of fees between physicians) and compérage [14] (coalition between health professionals) are banned.

A physician, medical practitioner, medical doctor, or simply doctor is a health professional who practices medicine, which is concerned with promoting, maintaining or restoring health through the study, diagnosis, prognosis and treatment of disease, injury, and other physical and mental impairments. Physicians may focus their practice on certain disease categories, types of patients, and methods of treatment—known as specialities—or they may assume responsibility for the provision of continuing and comprehensive medical care to individuals, families, and communities—known as general practice. Medical practice properly requires both a detailed knowledge of the academic disciplines, such as anatomy and physiology, underlying diseases, and their treatment, which is the science of medicine, and a decent competence in its applied practice, which is the art or craft of the profession.

Emergency medicine is the medical speciality concerned with the care of illnesses or injuries requiring immediate medical attention. Emergency medicine physicians specialize in providing care for unscheduled and undifferentiated patients of all ages. As first-line providers, in coordination with emergency medical services, they are primarily responsible for initiating resuscitation and stabilization and performing the initial investigations and interventions necessary to diagnose and treat illnesses or injuries in the acute phase. Emergency medical physicians generally practice in hospital emergency departments, pre-hospital settings via emergency medical services, and intensive care units. Still, they may also work in primary care settings such as urgent care clinics.
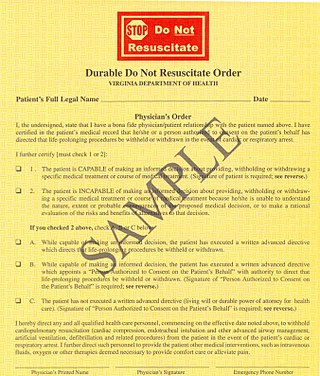
A do-not-resuscitate order (DNR), also known as Do Not Attempt Resuscitation (DNAR), Do Not Attempt Cardiopulmonary Resuscitation (DNACPR), no code or allow natural death, is a medical order, written or oral depending on the jurisdiction, indicating that a person should not receive cardiopulmonary resuscitation (CPR) if that person's heart stops beating. Sometimes these decisions and the relevant documents also encompass decisions around other critical or life-prolonging medical interventions. The legal status and processes surrounding DNR orders vary in different polities. Most commonly, the order is placed by a physician based on a combination of medical judgement and patient involvement.

A general practitioner (GP) or family physician is a doctor who is a consultant in general practice.
Osteopathic medicine is a branch of the medical profession in the United States that promotes the practice of science-based medicine, often referred to in this context as allopathic medicine, with a set of philosophy and principles set by its earlier form, osteopathy. Osteopathic physicians (DOs) are graduates of American osteopathic medical colleges and are licensed to practice the full scope of medicine and surgery in all 50 U.S. states. The field is distinct from osteopathic practices offered in nations outside of the U.S.—in which practitioners are generally considered neither parts of core medical staff nor of medicine itself; rather, they are considered alternative medicine practitioners. The other major branch of medicine in the United States is referred to by practitioners of osteopathic medicine as allopathic medicine.
Internal medicine, also known as general internal medicine in Commonwealth nations, is a medical specialty for medical doctors focused on the prevention, diagnosis, and treatment of internal diseases in adults. Medical practitioners of internal medicine are referred to as internists, or physicians in Commonwealth nations. Internists possess specialized skills in managing patients with undifferentiated or multi-system disease processes. They provide care to both hospitalized (inpatient) and ambulatory (outpatient) patients and often contribute significantly to teaching and research. Internists are qualified physicians who have undergone postgraduate training in internal medicine, and should not be confused with "interns", a term commonly used for a medical doctor who has obtained a medical degree but does not yet have a license to practice medicine unsupervised.
Medical ethics is an applied branch of ethics which analyzes the practice of clinical medicine and related scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. These values include the respect for autonomy, non-maleficence, beneficence, and justice. Such tenets may allow doctors, care providers, and families to create a treatment plan and work towards the same common goal. These four values are not ranked in order of importance or relevance and they all encompass values pertaining to medical ethics. However, a conflict may arise leading to the need for hierarchy in an ethical system, such that some moral elements overrule others with the purpose of applying the best moral judgement to a difficult medical situation. Medical ethics is particularly relevant in decisions regarding involuntary treatment and involuntary commitment.

The American Medical Association (AMA) is an American professional association and lobbying group of physicians and medical students. Founded in 1847, it is headquartered in Chicago, Illinois. Membership was 271,660 in 2022.

Primary care is a model of health care that supports first-contact, accessible, continuous, comprehensive and coordinated person-focused care. It aims to optimise population health and reduce disparities across the population by ensuring that subgroups have equal access to services.
The term managed care or managed healthcare is used in the United States to describe a group of activities intended to reduce the cost of providing health care and providing American health insurance while improving the quality of that care. It has become the predominant system of delivering and receiving American health care since its implementation in the early 1980s, and has been largely unaffected by the Affordable Care Act of 2010.
...intended to reduce unnecessary health care costs through a variety of mechanisms, including: economic incentives for physicians and patients to select less costly forms of care; programs for reviewing the medical necessity of specific services; increased beneficiary cost sharing; controls on inpatient admissions and lengths of stay; the establishment of cost-sharing incentives for outpatient surgery; selective contracting with health care providers; and the intensive management of high-cost health care cases. The programs may be provided in a variety of settings, such as Health Maintenance Organizations and Preferred Provider Organizations.
The Joint Commission is a United States-based nonprofit tax-exempt 501(c) organization that accredits more than 22,000 US health care organizations and programs. The international branch accredits medical services from around the world.

Family medicine is a medical specialty within primary care that provides continuing and comprehensive health care for the individual and family across all ages, genders, diseases, and parts of the body. The specialist, who is usually a primary care physician, is named a family physician. It is often referred to as general practice and a practitioner as a general practitioner. Historically, their role was once performed by any doctor with qualifications from a medical school and who works in the community. However, since the 1950s, family medicine / general practice has become a specialty in its own right, with specific training requirements tailored to each country. The names of the specialty emphasize its holistic nature and/or its roots in the family. It is based on knowledge of the patient in the context of the family and the community, focusing on disease prevention and health promotion. According to the World Organization of Family Doctors (WONCA), the aim of family medicine is "promoting personal, comprehensive and continuing care for the individual in the context of the family and the community". The issues of values underlying this practice are usually known as primary care ethics.
In the healthcare industry, pay for performance (P4P), also known as "value-based purchasing", is a payment model that offers financial incentives to physicians, hospitals, medical groups, and other healthcare providers for meeting certain performance measures. Clinical outcomes, such as longer survival, are difficult to measure, so pay for performance systems usually evaluate process quality and efficiency, such as measuring blood pressure, lowering blood pressure, or counseling patients to stop smoking. This model also penalizes health care providers for poor outcomes, medical errors, or increased costs. Integrated delivery systems where insurers and providers share in the cost are intended to help align incentives for value-based care.
Fee-for-service (FFS) is a payment model where services are unbundled and paid for separately.
The French health care system is one of universal health care largely financed by government national health insurance. In its 2000 assessment of world health care systems, the World Health Organization found that France provided the "best overall health care" in the world. In 2017, France spent 11.3% of GDP on health care, or US$5,370 per capita, a figure higher than the average spent by rich countries, though similar to Germany (10.6%) and Canada (10%), but much less than in the US. Approximately 77% of health expenditures are covered by government funded agencies.
An accountable care organization (ACO) is a healthcare organization that ties provider reimbursements to quality metrics and reductions in the cost of care. ACOs in the United States are formed from a group of coordinated health-care practitioners. They use alternative payment models, normally, capitation. The organization is accountable to patients and third-party payers for the quality, appropriateness and efficiency of the health care provided. According to the Centers for Medicare and Medicaid Services, an ACO is "an organization of health care practitioners that agrees to be accountable for the quality, cost, and overall care of Medicare beneficiaries who are enrolled in the traditional fee-for-service program who are assigned to it".
The Center for Personalized Education for Physicians (CPEP) is a non-profit organization, headquartered in Denver, Colorado, and it specializes in physician competency assessment and educational intervention. The organization was established in 1990 as a collaborative effort of seven Colorado healthcare organizations: the Colorado Alliance for CME, the Colorado Foundation for Medical Care, the Colorado Hospital Association, the Colorado Medical Society, the Colorado Physician Health Program, the Colorado Society of Osteopathic Medicine and the University of Colorado School of Medicine.
Primary care ethics is the study of the everyday decisions that primary care clinicians make, such as: how long to spend with a particular patient, how to reconcile their own values and those of their patients, when and where to refer or investigate, how to respect confidentiality when dealing with patients, relatives and third parties. All these decisions involve values as well as facts and are therefore ethical issues. These issues may also involve other workers in primary healthcare, such as receptionists and managers.
Conflict of interest in the health care industry occurs when the primary goal of protecting and increasing the health of patients comes into conflict with any other secondary goal, especially personal gain to healthcare professionals, and increasing revenue to a healthcare organization from selling health care products and services. The public and private sectors of the medical-industrial complex have various conflicts of interest which are specific to these entities.

Physicians and surgeons play an important role in the provision of health care in Canada. They are responsible for the promotion, maintenance, and restoration of health through the study, diagnosis, prognosis, and treatment of disease, injury, and other physical and mental impairments. As Canadian medical schools solely offer the Doctor of Medicine (M.D.) or Doctor of Medicine and Master of Surgery degrees, these represent the degrees held by the vast majority of physicians and surgeons in Canada, though some have a Doctor of Osteopathic Medicine (D.O.) from the United States or Bachelor of Medicine, Bachelor of Surgery from Europe.