Related Research Articles

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

The occipital bone is a cranial dermal bone and the main bone of the occiput. It is trapezoidal in shape and curved on itself like a shallow dish. The occipital bone overlies the occipital lobes of the cerebrum. At the base of the skull in the occipital bone, there is a large oval opening called the foramen magnum, which allows the passage of the spinal cord.

Obstetric ultrasonography, or prenatal ultrasound, is the use of medical ultrasonography in pregnancy, in which sound waves are used to create real-time visual images of the developing embryo or fetus in the uterus (womb). The procedure is a standard part of prenatal care in many countries, as it can provide a variety of information about the health of the mother, the timing and progress of the pregnancy, and the health and development of the embryo or fetus.

Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible. These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts or as early in gestation as practicable. Screening can detect problems such as neural tube defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Down syndrome, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems which primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.
Oligohydramnios is a medical condition in pregnancy characterized by a deficiency of amniotic fluid, the fluid that surrounds the fetus in the abdomen, in the amniotic sac. It is typically diagnosed by ultrasound when the amniotic fluid index (AFI) measures less than 5 cm or when the single deepest pocket (SDP) of amniotic fluid measures less than 2 cm. Amniotic fluid is necessary to allow for normal fetal movement, lung development, and cushioning from uterine compression. Low amniotic fluid can be attributed to a maternal, fetal, placental or idiopathic cause and can result in poor fetal outcomes including death. The prognosis of the fetus is dependent on the etiology, gestational age at diagnosis, and the severity of the oligohydramnios.

The nasal septum separates the left and right airways of the nasal cavity, dividing the two nostrils.

The gestational sac is the large cavity of fluid surrounding the embryo. During early embryogenesis it consists of the extraembryonic coelom, also called the chorionic cavity. The gestational sac is normally contained within the uterus. It is the only available structure that can be used to determine if an intrauterine pregnancy exists until the embryo can be identified.

A blighted ovum is a pregnancy in which the embryo never develops or develops and is reabsorbed. In a normal pregnancy, an embryo would be visible on an ultrasound by six weeks after the woman's last menstrual period. Anembryonic gestation is one of the causes of miscarriage of a pregnancy.
In obstetrics, gestational age is a measure of the age of a pregnancy taken from the beginning of the woman's last menstrual period (LMP), or the corresponding age of the gestation as estimated by a more accurate method if available. Such methods include adding 14 days to a known duration since fertilization, or by obstetric ultrasonography. The popularity of using this measure of pregnancy is due to the fact that menstrual periods are usually noticed, while there is generally no convenient way to discern when fertilization or implantation occurred. Gestational age is contrasted with fertilization age which takes the date of fertilization as the start date of gestation, and pregnancy which begins with implantation.

The chordae tendineae (tendinous cords), colloquially known as the heart strings, are inelastic cords of fibrous connective tissue that connect the papillary muscles to the tricuspid valve and the mitral valve in the heart.
Postterm pregnancy is when a woman has not yet delivered her baby after 42 weeks of gestation, two weeks beyond the typical 40-week duration of pregnancy. Postmature births carry risks for both the mother and the baby, including fetal malnutrition, meconium aspiration syndrome, and stillbirths. After the 42nd week of gestation, the placenta, which supplies the baby with nutrients and oxygen from the mother, starts aging and will eventually fail. Postterm pregnancy is a reason to induce labor.

A nuchal scan or nuchal translucency (NT) scan/procedure is a sonographic prenatal screening scan (ultrasound) to detect chromosomal abnormalities in a fetus, though altered extracellular matrix composition and limited lymphatic drainage can also be detected.
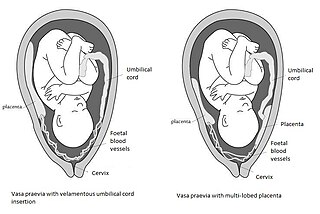
Vasa praevia is a condition in which fetal blood vessels cross or run near the internal opening of the uterus. These vessels are at risk of rupture when the supporting membranes rupture, as they are unsupported by the umbilical cord or placental tissue.
Fetal movement refers to motion of a fetus caused by its own muscle activity. Locomotor activity begins during the late embryological stage and changes in nature throughout development. Muscles begin to move as soon as they are innervated. These first movements are not reflexive, but arise from self-generated nerve impulses originating in the spinal cord. As the nervous system matures, muscles can move in response to stimuli.
A Doppler fetal monitor is a hand-held ultrasound transducer used to detect the fetal heartbeat for prenatal care. It uses the Doppler effect to provide an audible simulation of the heart beat. Some models also display the heart rate in beats per minute (BPM). Use of this monitor is sometimes known as Doppler auscultation. The Doppler fetal monitor is commonly referred to simply as a Doppler or fetal Doppler. It may be classified as a form of Doppler ultrasonography.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.

Monoamniotic twins are identical or semi-identical twins that share the same amniotic sac within their mother's uterus. Monoamniotic twins are always monochorionic and are usually termed Monoamniotic-Monochorionic twins. They share the placenta, but have two separate umbilical cords. Monoamniotic twins develop when an embryo does not split until after formation of the amniotic sac, at about 9–13 days after fertilization. Monoamniotic triplets or other monoamniotic multiples are possible, but extremely rare. Other obscure possibilities include multiples sets where monoamniotic twins are part of a larger gestation such as triplets, quadruplets, or more.

A six-week abortion ban or early abortion ban, called a "heartbeat bill" or "fetal heartbeat bill" by proponents, is a form of abortion restriction legislation in the United States. These bans make abortion illegal as early as six weeks gestational age, which is when proponents claim that a "fetal heartbeat" can be detected. Medical and reproductive health experts, including the American Medical Association and the American College of Obstetricians and Gynecologists, say that the reference to a fetal heartbeat is medically inaccurate and intentionally misleading because a conceptus is not called a fetus until after ten weeks of pregnancy, before which the proper term is an embryo, as well as that at six weeks the embryo has no heart, which at that stage is only a group of cells which will become a heart. Medical professionals advise that a true fetal heartbeat cannot be detected until around 17 to 20 weeks of gestation when the chambers of the heart have become sufficiently developed.
Foetal cerebral redistribution or 'brain-sparing' is a diagnosis in foetal medicine. It is characterised by preferential flow of blood towards the brain at the expense of the other vital organs, and it occurs as a haemodynamic adaptation in foetuses which have placental insufficiency. The underlying mechanism is thought to be vasodilation of the cerebral arteries. Cerebral redistribution is defined by the presence of a low middle cerebral artery pulsatility index (MCA-PI). Ultrasound of the middle cerebral artery to examine the Doppler waveform is used to establish this. Although cerebral redistribution represents an effort to preserve brain development in the face of hypoxic stress, it is nonetheless associated with adverse neurodevelopmental outcome. The presence of cerebral redistribution will be one factor taken into consideration when deciding whether to artificially deliver a baby with placental insufficiency via induction of labour or caesarian section.
The anomaly scan, also sometimes called the anatomy scan, 20-week ultrasound, or level 2 ultrasound, evaluates anatomic structures of the fetus, placenta, and maternal pelvic organs. This scan is an important and common component of routine prenatal care. The function of the ultrasound is to measure the fetus so that growth abnormalities can be recognized quickly later in pregnancy, to assess for congenital malformations and multiple pregnancies, and to plan method of delivery.
References
- ↑ "Fetal pole | Radiology Reference Article | Radiopaedia.org". radiopaedia.org.