Related Research Articles

Dementia is the general name for a decline in cognitive abilities that impacts a person's ability to perform everyday activities. This typically involves problems with memory, thinking, and behavior. Aside from memory impairment and a disruption in thought patterns, the most common symptoms include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Dementia ultimately has a significant effect on the individual, caregivers, and on social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than what is caused by normal aging.

Parkinsonism is a clinical syndrome characterized by tremor, bradykinesia, rigidity, and postural instability. These are the four motor symptoms found in Parkinson's disease (PD) – after which it is named – dementia with Lewy bodies (DLB), Parkinson's disease dementia (PDD), and many other conditions. This set of symptoms occurs in a wide range of conditions and may have many causes, including neurodegenerative conditions, drugs, toxins, metabolic diseases, and neurological conditions other than PD.

Dementia with Lewy bodies (DLB) is a type of dementia characterized by changes in sleep, behavior, cognition, movement, and regulation of automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive impairment interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the prevalence is not known accurately and many diagnoses are missed. The disease was first described by Kenji Kosaka in 1976.
Vascular dementia (VaD) is dementia caused by problems in the blood supply to the brain, resulting from a cerebrovascular disease. Restricted blood supply (ischemia) leads to cell and tissue death in the affected region, known as an infarct. The three types of vascular dementia are subcortical vascular dementia, multi-infarct dementia, and stroke related dementia. Subcortical vascular dementia is brought about by damage to the small blood vessels in the brain. Multi-infarct dementia is brought about by a series of mini-strokes where many regions have been affected. The third type is stroke related where more serious damage may result. Such damage leads to varying levels of cognitive decline. When caused by mini-strokes, the decline in cognition is gradual. When due to a stroke, the cognitive decline can be traced back to the event.
Lewy body dementias are two similar and common subtypes of dementia: Dementia with Lewy bodies (DLB) and Parkinson's disease dementia (PDD). Both are characterized by changes in thinking, movement, behavior, and mood. The two conditions have similar features and may have similar causes, and are believed to belong on a spectrum of Lewy body disease that includes Parkinson's disease. As of 2014, they were more often misdiagnosed than any other common dementia.

Frontotemporal dementia (FTD), or frontotemporal degeneration disease, or frontotemporal neurocognitive disorder, encompasses several types of dementia involving the progressive degeneration of frontal and temporal lobes. FTDs broadly present as behavioral or language disorders with gradual onsets. Common signs and symptoms include significant changes in social and personal behavior, apathy, blunting of emotions, and deficits in both expressive and receptive language. Currently, there is no cure for FTD, but there are treatments that help alleviate symptoms.
Cognitive disorders (CDs), also known as neurocognitive disorders (NCDs), are a category of mental health disorders that primarily affect cognitive abilities including learning, memory, perception, and problem-solving. Neurocognitive disorders include delirium, mild neurocognitive disorders, and major neurocognitive disorder. They are defined by deficits in cognitive ability that are acquired, typically represent decline, and may have an underlying brain pathology. The DSM-5 defines six key domains of cognitive function: executive function, learning and memory, perceptual-motor function, language, complex attention, and social cognition.
The mini–mental state examination (MMSE) or Folstein test is a 30-point questionnaire that is used extensively in clinical and research settings to measure cognitive impairment. It is commonly used in medicine and allied health to screen for dementia. It is also used to estimate the severity and progression of cognitive impairment and to follow the course of cognitive changes in an individual over time; thus making it an effective way to document an individual's response to treatment. The MMSE's purpose has been not, on its own, to provide a diagnosis for any particular nosological entity.
Cognitive impairment is an inclusive term to describe any characteristic that acts as a barrier to the cognition process or different areas of cognition. Cognition, also known as cognitive function, refers to the mental processes of how a person gains knowledge, uses existing knowledge, and understands things that are happening around them using their thoughts and senses. A cognitive impairment can be in different domains or aspects of a person's cognitive function including memory, attention span, planning, reasoning, decision-making, language, executive functioning, and visuospatial functioning. The term cognitive impairment covers many different diseases and conditions and may also be symptom or manifestation of a different underlying condition. Examples include impairments in overall intelligence ,specific and restricted impairments in cognitive abilities, neuropsychological impairments, or it may describe drug-induced impairment in cognition and memory. Cognitive impairments may be short-term, progressive or permanent.
In medicine, a prodrome is an early sign or symptom that often indicates the onset of a disease before more diagnostically specific signs and symptoms develop. It is derived from the Greek word prodromos, meaning "running before". Prodromes may be non-specific symptoms or, in a few instances, may clearly indicate a particular disease, such as the prodromal migraine aura.

Alzheimer's disease (AD) is a neurodegenerative disease that usually starts slowly and progressively worsens, and is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in remembering recent events. As the disease advances, symptoms can include problems with language, disorientation, mood swings, loss of motivation, self-neglect, and behavioral issues. As a person's condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the typical life expectancy following diagnosis is three to nine years.
The CDR computerized assessment system is a computerized battery of cognitive tests designed in the late 1970s by Professor Keith Wesnes at the University of Reading in Berkshire, England, for repeated testing in clinical trials. Task stimuli are presented in a laptop computer and participants respond via 'YES' and 'NO' buttons on a two-button response box, which records both the accuracy and reaction time.

Parkinson's disease (PD), or simply Parkinson's, is a chronic degenerative disorder of the central nervous system that affects both the motor system and non-motor systems. The symptoms usually emerge slowly, and as the disease worsens, non-motor symptoms become more common. Early symptoms are tremor, rigidity, slowness of movement, and difficulty with walking. Problems may also arise with cognition, behaviour, sleep, and sensory systems. Parkinson's disease dementia becomes common in advanced stages of the disease.
The applause sign is a behavioural indicator, relevant to neurodegenerative conditions, characterised by a patient’s inability to execute the same number of hand claps as demonstrated by an examiner.
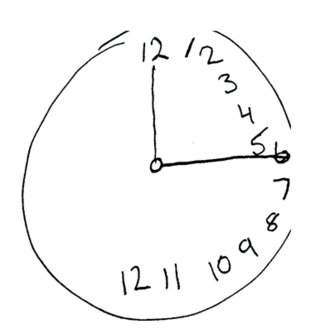
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.
Florbetaben, a fluorine-18 (18F)-labeled stilbene derivative, trade name NeuraCeq, is a diagnostic radiotracer developed for routine clinical application to visualize β-amyloid plaques in the brain. It is indicated for Positron Emission Tomography (PET) imaging of β-amyloid neuritic plaque density in the brains of adult patients with cognitive impairment who are being evaluated for Alzheimer's disease (AD) and other causes of cognitive impairment. β-amyloid is a key neuropathological hallmark of AD, so markers of β-amyloid plaque accumulation in the brain are useful in distinguishing AD from other causes of dementia. The tracer successfully completed a global multicenter phase 0–III development program and obtained approval in Europe, US and South Korea in 2014.
The mini-SEA is a neuropsychological battery aiming to evaluate the impairment of the social and emotional cognition. Developed by Maxime Bertoux in 2012, the mini-SEA has been preferentially designed for the assessment, follow-up and diagnosis of neurodegenerative diseases such as the frontotemporal dementia, but is more generally designed to evaluate the integrity of the frontal lobes.
Parkinson's disease dementia (PDD) is dementia that is associated with Parkinson's disease (PD). Together with dementia with Lewy bodies (DLB), it is one of the Lewy body dementias characterized by abnormal deposits of Lewy bodies in the brain.
The Dementia with Lewy Bodies Consortium is an international multidisciplinary collaboration of researchers interested in the dementia with Lewy bodies. It first convened in Newcastle upon Tyne, England, in October 1995. Between 1995 and 2005, it issued three DLBC Consensus Reports on dementia with Lewy bodies.
Corticobasal syndrome (CBS) is a rare, progressive atypical Parkinsonism syndrome and is a tauopathy related to frontotemporal dementia. CBS is typically caused by the deposit of tau proteins forming in different areas of the brain.
References
- ↑ Dubois B, Slachevsky A, Litvan I, Pillon B (December 2000). "The FAB: a Frontal Assessment Battery at bedside". Neurology. 55 (11): 1621–6. doi:10.1212/wnl.55.11.1621. PMID 11113214. S2CID 8973171.
- 1 2 3 Moreira HS, Costa AS, Castro SL, Lima CF, Vicente SG (2017). "Assessing Executive Dysfunction in Neurodegenerative Disorders: A Critical Review of Brief Neuropsychological Tools". Front Aging Neurosci (Review). 9: 369. doi: 10.3389/fnagi.2017.00369 . PMC 5684643 . PMID 29170636.
- ↑ Hurtado-Pomares M, Carmen Terol-Cantero M, Sánchez-Pérez A, Peral-Gómez P, Valera-Gran D, Navarrete-Muñoz EM (February 2018). "The frontal assessment battery in clinical practice: a systematic review". Int J Geriatr Psychiatry (Review). 33 (2): 237–251. doi:10.1002/gps.4751. PMID 28627719. S2CID 28971287.
- ↑ Kosaka K, ed. (2017). Dementia with Lewy bodies: clinical and biological aspects (1st ed.). Japan: Springer. pp. 75–76. doi:10.1007/978-4-431-55948-1. ISBN 978-4-431-55948-1. S2CID 45950966.