Hypochondriasis or hypochondria is a condition in which a person is excessively and unduly worried about having a serious illness. Hypochondria is an old concept whose meaning has repeatedly changed over its lifespan. It has been claimed that this debilitating condition results from an inaccurate perception of the condition of body or mind despite the absence of an actual medical diagnosis. An individual with hypochondriasis is known as a hypochondriac. Hypochondriacs become unduly alarmed about any physical or psychological symptoms they detect, no matter how minor the symptom may be, and are convinced that they have, or are about to be diagnosed with, a serious illness.

Obsessive–compulsive personality disorder (OCPD) is a cluster C personality disorder marked by a spectrum of obsessions with rules, lists, schedules, and order, among other things. Symptoms are usually present by the time a person reaches adulthood, and are visible in a variety of situations. The cause of OCPD is thought to involve a combination of genetic and environmental factors, namely problems with attachment.

Hoarding disorder (HD) or Plyushkin's disorder, is a mental disorder characterised by persistent difficulty in parting with possessions and engaging in excessive acquisition of items that are not needed or for which no space is available. This results in severely cluttered living spaces, distress, and impairment in personal, family, social, educational, occupational, or other important areas of functioning. Excessive acquisition is characterized by repetitive urges or behaviours related to amassing or buying property. Difficulty discarding possessions is characterized by a perceived need to save items and distress associated with discarding them. Accumulation of possessions results in living spaces becoming cluttered to the point that their use or safety is compromised. It is recognised by the eleventh revision of the International Classification of Diseases (ICD-11) and the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).
Scrupulosity is the pathological guilt/anxiety about moral or religious issues. Although it can affect nonreligious people, it is usually related to religious beliefs. It is personally distressing, dysfunctional, and often accompanied by significant impairment in social functioning. It is typically conceptualized as a moral or religious form of obsessive–compulsive disorder (OCD), The term is derived from the Latin scrupus, a sharp stone, implying a stabbing pain on the conscience. Scrupulosity was formerly called scruples in religious contexts, but the word scruple now commonly refers to a troubling of the conscience rather than to the disorder.
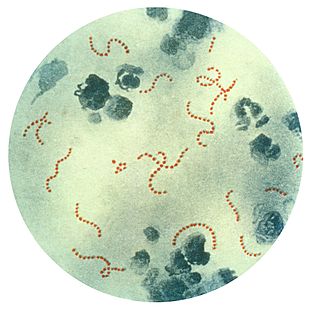
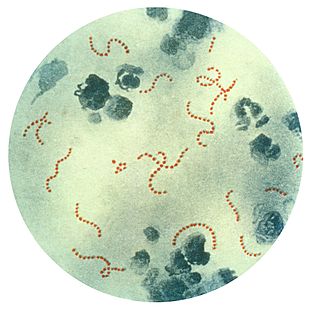
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) is a controversial hypothetical diagnosis for a subset of children with rapid onset of obsessive-compulsive disorder (OCD) or tic disorders. Symptoms are proposed to be caused by group A streptococcal (GAS), and more specifically, group A beta-hemolytic streptococcal (GABHS) infections. OCD and tic disorders are hypothesized to arise in a subset of children as a result of a post-streptococcal autoimmune process. The proposed link between infection and these disorders is that an autoimmune reaction to infection produces antibodies that interfere with basal ganglia function, causing symptom exacerbations, and this autoimmune response results in a broad range of neuropsychiatric symptoms.
The Yale–Brown Obsessive–Compulsive Scale (Y-BOCS) is a test to rate the severity of obsessive–compulsive disorder (OCD) symptoms.
The obsessive–compulsive spectrum is a model of medical classification where various psychiatric, neurological and/or medical conditions are described as existing on a spectrum of conditions related to obsessive–compulsive disorder (OCD). "The disorders are thought to lie on a spectrum from impulsive to compulsive where impulsivity is said to persist due to deficits in the ability to inhibit repetitive behavior with known negative consequences, while compulsivity persists as a consequence of deficits in recognizing completion of tasks." OCD is a mental disorder characterized by obsessions and/or compulsions. An obsession is defined as "a recurring thought, image, or urge that the individual cannot control". Compulsion can be described as a "ritualistic behavior that the person feels compelled to perform". The model suggests that many conditions overlap with OCD in symptomatic profile, demographics, family history, neurobiology, comorbidity, clinical course and response to various pharmacotherapies. Conditions described as being on the spectrum are sometimes referred to as obsessive–compulsive spectrum disorders.
Sexual obsessions are persistent and unrelenting thoughts about sexual activity. In the context of obsessive-compulsive disorder (OCD), these are extremely common, and can become extremely debilitating, making the person ashamed of the symptoms and reluctant to seek help. A preoccupation with sexual matters, however, does not only occur as a symptom of OCD, they may be enjoyable in other contexts.
Primarily obsessional obsessive–compulsive disorder, also known as purely obsessional obsessive–compulsive disorder, is a lesser-known form or manifestation of OCD. It is not a diagnosis in the DSM-5. For people with primarily obsessional OCD, there are fewer observable compulsions, compared to those commonly seen with the typical form of OCD. While ritualizing and neutralizing behaviors do take place, they are mostly cognitive in nature, involving mental avoidance and excessive rumination. Primarily obsessional OCD takes the form of intrusive thoughts often of a distressing, sexual, or violent nature.

Obsessive–compulsive disorder (OCD) is a mental and behavioral disorder in which an individual has intrusive thoughts and feels the need to perform certain routines (compulsions) repeatedly to relieve the distress caused by the obsession, to the extent where it impairs general function.
The cause of obsessive–compulsive disorder is understood mainly through identifying biological risk factors that lead to obsessive–compulsive disorder (OCD) symptomology. The leading hypotheses propose the involvement of the orbitofrontal cortex, basal ganglia, and/or the limbic system, with discoveries being made in the fields of neuroanatomy, neurochemistry, neuroimmunology, neurogenetics, and neuroethology.
In psychology, relationship obsessive–compulsive disorder (ROCD) is a form of obsessive–compulsive disorder focusing on close or intimate relationships. Such obsessions can become extremely distressing and debilitating, having negative impacts on relationships functioning.
The delayed-maturation theory of obsessive–compulsive disorder suggests that obsessive–compulsive disorder (OCD) can be caused by delayed maturation of the frontal striatal circuitry or parts of the brain that make up the frontal cortex, striatum, or integrating circuits. Some researchers suspect that variations in the volume of specific brain structures can be observed in children that have OCD. It has not been determined if delayed-maturation of this frontal circuitry contributes to the development of OCD or if OCD is the ailment that inhibits normal growth of structures in the frontal striatal, frontal cortex, or striatum. However, the use of neuroimaging has equipped researchers with evidence of some brain structures that are consistently less adequate and less matured in patients diagnosed with OCD in comparison to brains without OCD. More specifically, structures such as the caudate nucleus, volumes of gray matter, white matter, and the cingulate have been identified as being less developed in people with OCD in comparison to individuals that do not have OCD. However, the cortex volume of the operculum (brain) is larger and OCD patients are also reported to have larger temporal lobe volumes; which has been identified in some women patients with OCD. Further research is needed to determine the effect of these structural size differences on the onset and degree of OCD and the maturation of specific brain structures.
The University of Florida Obsessive–Compulsive Disorder Program is a treatment and research clinic in the Department of Psychiatry at the University of Florida. The clinic is located in Gainesville, Florida.
Daniel A. Geller is an Australian American pediatrician and psychiatrist who specializes in the treatment of pediatric obsessive–compulsive disorder (OCD). Geller is triple board certified in Pediatrics, Psychiatry, and Child & Adolescent Psychiatry, and is director of the Pediatric OCD Program at Massachusetts General Hospital.

Wayne Goodman is an American psychiatrist and researcher who specializes in Obsessive-Compulsive Disorder (OCD). He is the principal developer, along with his colleagues, of the Yale-Brown Obsessive Compulsive Scale (Y-BOCS).

Jonathan Stuart Abramowitz is an American clinical psychologist and Professor in the Department of Psychology and Neuroscience at the University of North Carolina at Chapel Hill (UNC-CH). He is an expert on obsessive-compulsive disorder (OCD) and anxiety disorders whose work is highly cited. He maintains a research lab and currently serves as the Director of the UNC-CH Clinical Psychology PhD Program. Abramowitz approaches the understanding and treatment of psychological problems from a cognitive-behavioral perspective.
The Dimensional Obsessive-Compulsive Scale (DOCS) is a 20-item self-report instrument that assesses the severity of Obsessive-Compulsive Disorder (OCD) symptoms along four empirically supported theme-based dimensions: (a) contamination, (b) responsibility for harm and mistakes, (c) incompleteness/symmetry, and (d) unacceptable (taboo) thoughts. The scale was developed in 2010 by a team of experts on OCD led by Jonathan Abramowitz, PhD to improve upon existing OCD measures and advance the assessment and understanding of OCD. The DOCS contains four subscales that have been shown to have good reliability, validity, diagnostic sensitivity, and sensitivity to treatment effects in a variety of settings cross-culturally and in different languages. As such, the DOCS meets the needs of clinicians and researchers who wish to measure current OCD symptoms or assess changes in symptoms over time.
John Piacentini, PhD, ABPP, is an American clinical child and adolescent psychologist, and professor of psychiatry and biobehavioral sciences at the David Geffen School of Medicine at UCLA in Los Angeles, California. He is the director of the Center for Child Anxiety, Resilience, Education and Support (CARES), and the Child OCD, Anxiety and Tic Disorders Program at UCLA's Semel Institute for Neuroscience and Human Behavior.
Inference-based therapy (IBT), also known as inference-based cognitive behavioral therapy (I-CBT), originated as a form of cognitive therapy developed for treating obsessive-compulsive disorder. IBT followed the observation that people with OCD often inferred danger on the basis of inverse inference. Later the model was extended to inferential confusion, where inverse inference leads to distrust of the senses and investment in remote possibility. In this model, individuals with obsessive-compulsive disorder are hypothesized to put a greater emphasis on an imagined possibility than on what can be perceived with the senses, and to confuse the imagined possibility with reality. According to inference-based therapy, obsessional thinking occurs when the person replaces reality and real probabilities with imagined possibilities; the obsession is hypothesized to concern a doubt about a possible state of affairs.