
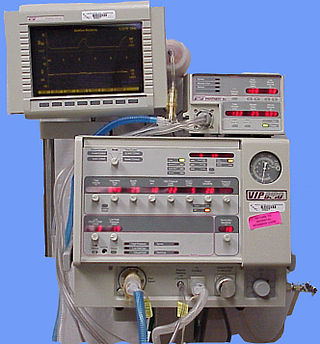
A ventilator is a type of breathing apparatus, a class of medical technology that provides mechanical ventilation by moving breathable air into and out of the lungs, to deliver breaths to a patient who is physically unable to breathe, or breathing insufficiently. Ventilators may be computerized microprocessor-controlled machines, but patients can also be ventilated with a simple, hand-operated bag valve mask. Ventilators are chiefly used in intensive-care medicine, home care, and emergency medicine and in anesthesiology.

Mechanical ventilation or assisted ventilation is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

An iron lung is a type of negative pressure ventilator (NPV), a mechanical respirator which encloses most of a person's body and varies the air pressure in the enclosed space to stimulate breathing. It assists breathing when muscle control is lost, or the work of breathing exceeds the person's ability. Need for this treatment may result from diseases including polio and botulism and certain poisons.
The control of ventilation is the physiological mechanisms involved in the control of breathing, which is the movement of air into and out of the lungs. Ventilation facilitates respiration. Respiration refers to the utilization of oxygen and balancing of carbon dioxide by the body as a whole, or by individual cells in cellular respiration.

Spirometry is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD. It is also helpful as part of a system of health surveillance, in which breathing patterns are measured over time.

Respiratory arrest is a serious medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.

A bag valve mask (BVM), sometimes known by the proprietary name Ambu bag or generically as a manual resuscitator or "self-inflating bag", is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately. The device is a required part of resuscitation kits for trained professionals in out-of-hospital settings (such as ambulance crews) and is also frequently used in hospitals as part of standard equipment found on a crash cart, in emergency rooms or other critical care settings. Underscoring the frequency and prominence of BVM use in the United States, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care recommend that "all healthcare providers should be familiar with the use of the bag-mask device." Manual resuscitators are also used within the hospital for temporary ventilation of patients dependent on mechanical ventilators when the mechanical ventilator needs to be examined for possible malfunction or when ventilator-dependent patients are transported within the hospital. Two principal types of manual resuscitators exist; one version is self-filling with air, although additional oxygen (O2) can be added but is not necessary for the device to function. The other principal type of manual resuscitator (flow-inflation) is heavily used in non-emergency applications in the operating room to ventilate patients during anesthesia induction and recovery.
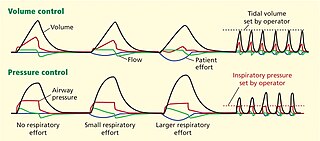
Dual-control modes of ventilation are auto-regulated pressure-controlled modes of mechanical ventilation with a user-selected tidal volume target. The ventilator adjusts the pressure limit of the next breath as necessary according to the previous breath's measured exhaled tidal volume. Peak airway pressure varies from breath to breath according to changes in the patient's airway resistance and lung compliance.
A wheeze is a clinical symptom of a continuous, coarse, whistling sound produced in the respiratory airways during breathing. For wheezes to occur, part of the respiratory tree must be narrowed or obstructed, or airflow velocity within the respiratory tree must be heightened. Wheezing is commonly experienced by persons with a lung disease; the most common cause of recurrent wheezing is asthma, though it can also be a symptom of lung cancer, congestive heart failure, and certain types of heart diseases.

An incentive spirometer is a handheld medical device used to help patients improve the functioning of their lungs. By training patients to take slow and deep breaths, this simplified spirometer facilitates lung expansion and strengthening. Patients inhale through a mouthpiece, which causes a piston inside the device to rise. This visual feedback helps them monitor their inspiratory effort. Incentive spirometers are commonly used after surgery or other illnesses to prevent pulmonary complications.

The respiratory center is located in the medulla oblongata and pons, in the brainstem. The respiratory center is made up of three major respiratory groups of neurons, two in the medulla and one in the pons. In the medulla they are the dorsal respiratory group, and the ventral respiratory group. In the pons, the pontine respiratory group includes two areas known as the pneumotaxic center and the apneustic center.
Pulmonary hygiene, also referred to as pulmonary toilet, is a set of methods used to clear mucus and secretions from the airways. The word pulmonary refers to the lungs. The word toilet, related to the French toilette, refers to body care and hygiene; this root is used in words such as toiletry that also relate to cleansing.
Pulmonary rehabilitation, also known as respiratory rehabilitation, is an important part of the management and health maintenance of people with chronic respiratory disease who remain symptomatic or continue to have decreased function despite standard medical treatment. It is a broad therapeutic concept. It is defined by the American Thoracic Society and the European Respiratory Society as an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities. In general, pulmonary rehabilitation refers to a series of services that are administered to patients of respiratory disease and their families, typically to attempt to improve the quality of life for the patient. Pulmonary rehabilitation may be carried out in a variety of settings, depending on the patient's needs, and may or may not include pharmacologic intervention.
Neurally adjusted ventilatory assist (NAVA) is a mode of mechanical ventilation. NAVA delivers assistance in proportion to and in synchrony with the patient's respiratory efforts, as reflected by an electrical signal. This signal represents the electrical activity of the diaphragm, the body's principal breathing muscle.
Pressure support ventilation (PSV), also known as pressure support, is a spontaneous mode of ventilation. The patient initiates every breath and the ventilator delivers support with the preset pressure value. With support from the ventilator, the patient also regulates their own respiratory rate and tidal volume.
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.
Continuous mandatory ventilation (CMV) is a mode of mechanical ventilation in which breaths are delivered based on set variables. Still used in the operating room, in previous nomenclature, CMV referred to "controlled mechanical ventilation", a mode of ventilation characterized by a ventilator that makes no effort to sense patient breathing effort. In continuous mandatory ventilation, the ventilator can be triggered either by the patient or mechanically by the ventilator. The ventilator is set to deliver a breath according to parameters selected by the operator. "Controlled mechanical ventilation" is an outdated expansion for "CMV"; "continuous mandatory ventilation" is now accepted standard nomenclature for mechanical ventilation. CMV today can assist or control itself dynamically, depending on the transient presence or absence of spontaneous breathing effort. Thus, today's CMV would have been called ACV in older nomenclature, and the original form of CMV is a thing of the past. But despite continual technological improvement over the past half century, CMV may still be uncomfortable for the patient.
Many terms are used in mechanical ventilation, some are specific to brand, model, trademark and mode of mechanical ventilation. There is a standardized nomenclature of mechanical ventilation that is specific about nomenclature related to modes, but not settings and variables.
Intermittent Mandatory Ventilation (IMV) refers to any mode of mechanical ventilation where a regular series of breaths are scheduled but the ventilator senses patient effort and reschedules mandatory breaths based on the calculated need of the patient. Similar to continuous mandatory ventilation in parameters set for the patients pressures and volumes but distinct in its ability to support a patient by either supporting their own effort or providing support when patient effort is not sensed. IMV is frequently paired with additional strategies to improve weaning from ventilator support or to improve cardiovascular stability in patients who may need full life support.
Rheotrauma is a medical term for the harm caused to a patient's lungs by high gas flows as delivered by mechanical ventilation. Although mechanical ventilation may prevent death of a patient from the hypoxia or hypercarbia which may be caused by respiratory failure, it can also be damaging to the lungs, leading to ventilator-associated lung injury. Rheotrauma is one of the ways in which mechanical ventilation may do this, alongside volutrauma, barotrauma, atelectotrauma and biotrauma. Attempts have been made to combine all of the mechanical forces caused by the ventilator on the patient's lungs in an all encompassing term: mechanical power.