Related Research Articles
Microangiopathic hemolytic anemia (MAHA) is a microangiopathic subgroup of hemolytic anemia caused by factors in the small blood vessels. It is identified by the finding of anemia and schistocytes on microscopy of the blood film.
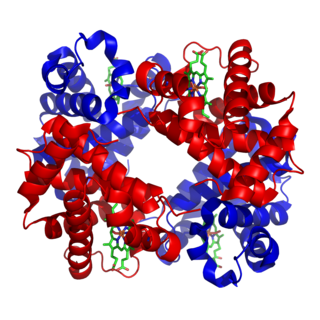
Glycosylphosphatidylinositol, or glycophosphatidylinositol, or GPI in short, is a phosphoglyceride that can be attached to the C-terminus of a protein during posttranslational modification. The resulting GPI-anchored proteins play key roles in a wide variety of biological processes. GPI is composed of a phosphatidylinositol group linked through a carbohydrate-containing linker and via an ethanolamine phosphate (EtNP) bridge to the C-terminal amino acid of a mature protein. The two fatty acids within the hydrophobic phosphatidyl-inositol group anchor the protein to the cell membrane.

Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired, life-threatening disease of the blood characterized by destruction of red blood cells by the complement system, a part of the body's innate immune system. This destructive process occurs due to deficiency of the red blood cell surface protein DAF, which normally inhibits such immune reactions. Since the complement cascade attacks the red blood cells within the blood vessels of the circulatory system, the red blood cell destruction (hemolysis) is considered an intravascular hemolytic anemia. Other key features of the disease, such as the high incidence of venous blood clot formation, are incompletely understood.

Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels or elsewhere in the human body (extravascular). This most commonly occurs within the spleen, but also can occur in the reticuloendothelial system or mechanically. Hemolytic anemia accounts for 5% of all existing anemias. It has numerous possible consequences, ranging from general symptoms to life-threatening systemic effects. The general classification of hemolytic anemia is either intrinsic or extrinsic. Treatment depends on the type and cause of the hemolytic anemia.
Hemoglobinuria is a condition in which the oxygen transport protein hemoglobin is found in abnormally high concentrations in the urine. The condition is caused by excessive intravascular hemolysis, in which large numbers of red blood cells (RBCs) are destroyed, thereby releasing free hemoglobin into the plasma. Excess hemoglobin is filtered by the kidneys, which excrete it into the urine, giving urine a purple color. Hemoglobinuria can lead to acute tubular necrosis which is an uncommon cause of a death of uni-traumatic patients recovering in the ICU.
A Coombs test, also known as antiglobulin test (AGT), is either of two blood tests used in immunohematology. They are the direct and indirect Coombs tests. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells. Since these antibodies sometimes destroy red blood cells, a person can be anemic and this test can help clarify the condition. The indirect Coombs detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells and the test can be done to diagnose reactions to a blood transfusion.
Autoimmune hemolytic anemia (AIHA) occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in the circulation. The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, with an incidence of 5–10 cases per 1 million persons per year in the warm-antibody type and 0.45 to 1.9 cases per 1 million persons per year in the cold antibody type. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.
Paroxysmal cold hemoglobinuria (PCH) is an autoimmune hemolytic anemia featured by complement-mediated intravascular hemolysis after cold exposure. It can present as an acute non-recurrent postinfectious event in children, or chronic relapsing episodes in adults with hematological malignancies or tertiary syphilis. Described by Julius Donath (1870–1950) and Karl Landsteiner (1868–1943) in 1904, PCH is one of the first clinical entities recognized as an autoimmune disorder.

Complement decay-accelerating factor, also known as CD55 or DAF, is a protein that, in humans, is encoded by the CD55 gene.

Eculizumab, sold under the brand name Soliris among others, is a medication used to treat paroxysmal nocturnal hemoglobinuria (PNH), atypical hemolytic uremic syndrome (aHUS), generalized myasthenia gravis, and neuromyelitis optica. In people with PNH, it reduces both the destruction of red blood cells and need for blood transfusion, but does not appear to affect the risk of death. Eculizumab was the first drug approved for each of its uses, and its approval was granted based on small trials. It is given in a clinic by intravenous (IV) infusion.

Phosphatidylinositol N-acetylglucosaminyltransferase subunit A is the catalytic subunit of the phosphatidylinositol N-acetylglucosaminyltransferase enzyme, which in humans is encoded by the PIGA gene.
Hematologic diseases are disorders which primarily affect the blood & blood-forming organs. Hematologic diseases include rare genetic disorders, anemia, HIV, sickle cell disease & complications from chemotherapy or transfusions.
Acquired hemolytic anemia can be divided into immune and non-immune mediated forms of hemolytic anemia.

In hematology, red cell agglutination or autoagglutination is a phenomenon in which red blood cells clump together, forming aggregates. It is caused by the surface of the red cells being coated with antibodies. This often occurs in cold agglutinin disease, a type of autoimmune hemolytic anemia in which people produce antibodies that bind to their red blood cells at cold temperatures and destroy them. People may develop cold agglutinins from lymphoproliferative disorders, from infection with Mycoplasma pneumoniae or Epstein–Barr virus, or idiopathically. Red cell agglutination can also occur in paroxysmal nocturnal hemoglobinuria and warm autoimmune hemolytic anemia. In cases of red cell agglutination, the direct antiglobulin test can be used to demonstrate the presence of antibodies bound to the red cells.
Fluorescein-labeled proaerolysin (FLAER) is used in a flow cytometric assay to diagnose paroxysmal nocturnal hemoglobinuria (PNH). The assay takes advantage of the action of proaerolysin, a prototoxin of aerolysin, a virulence factor of the bacterium Aeromonas hydrophila. Proaerolysin binds to the glycophosphatidylinositol(GPI) anchor in the plasma membrane of cells. Cells affected by PNH lack GPI anchoring proteins, and thus are not bound by proaerolysin. Of note, the FLAER-based assay is not suitable for evaluation of erythrocytes and platelets in PNH but flow cytometry assays based on CD55, CD59 and others are suitable.
Ravulizumab, sold under the brand name Ultomiris, is a humanized monoclonal antibody complement inhibitor medication designed for the treatment of paroxysmal nocturnal hemoglobinuria (PNH) and atypical hemolytic uremic syndrome. It is designed to bind to and prevent the activation of Complement component 5 (C5).
Donath–Landsteiner hemolytic anemia (DLHA) is a result of cold-reacting antibody immunoglobulin (Ig) induced hemolytic response inside vessels leading to anemia and, thus, a cold antibody autoimmune hemolytic anemias (CAAHA).
Pig-a gene mutation assay is a flow cytometry-based method for detecting mammalian cells that have inactivating mutations in the endogenous X-linked reporter gene called phosphatidyl inositolglycan class A gene. PIG-A is involved in the synthesis of glycosylphosphatidylinositol (GPI), an anchor molecule that tethers multiple protein marker molecules at the surface of the cells. When the sample containing wild-type and PIG-A mutant cells is labeled with fluorescent antibodies raised against GPI-anchored protein markers the wild-type cells will fluoresce and PIG-A mutant cells will not. The fraction of non-fluorescent PIG-A mutant cells in the antibody-labeled sample can be efficiently determined on any of the modern high throughput flow cytometers. The PIG-A mutant frequency fraction can be determined with high accuracy within minutes by processing samples containing a total of a million cells or more.
Pegcetacoplan, sold under the brand name Empaveli among others, is a medication used to treat paroxysmal nocturnal hemoglobinuria (PNH).

Iptacopan (LNP023) is a drug developed by Novartis designed to treat paroxysmal nocturnal hemoglobinuria (PNH), a disease in which the innate immune system destroys red blood cells. It is the first drug that selectively inhibits factor B, the active component of the complement's C3 and C5 convertases. In contrast to other PNH treatments like eculizumab, iptacopan is a small molecule.
References
- ↑ Ham, Thomas H. (1937). "Chronic Hemolytic Anemia with Paroxysmal Nocturnal Hemoglobinuria". New England Journal of Medicine. 217 (23): 915–7. doi:10.1056/NEJM193712022172307.
- ↑ MedlinePlus Encyclopedia : Ham test
- ↑ "Paroxysmal Nocturnal Hemoglobinuria - PNH". ARUP.
- ↑ Ferri, Fred F. (2015). Ferri's Clinical Advisor 2016 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 140. ISBN 9780323378222.