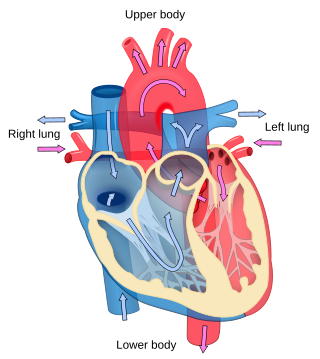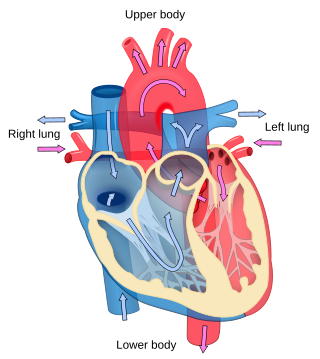
Cardiology is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a sub-specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.

A simulation is an imitative representation of a process or system that could exist in the real world. In this broad sense, simulation can often be used interchangeably with model. Sometimes a clear distinction between the two terms is made, in which simulations require the use of models; the model represents the key characteristics or behaviors of the selected system or process, whereas the simulation represents the evolution of the model over time. Another way to distinguish between the terms is to define simulation as experimentation with the help of a model. This definition includes time-independent simulations. Often, computers are used to execute the simulation.

Aortic regurgitation (AR), also known as aortic insufficiency (AI), is the leaking of the aortic valve of the heart that causes blood to flow in the reverse direction during ventricular diastole, from the aorta into the left ventricle. As a consequence, the cardiac muscle is forced to work harder than normal.

A cardiac stress test is a cardiological examination that evaluates the cardiovascular system's response to external stress within a controlled clinical setting. This stress response can be induced through physical exercise or intravenous pharmacological stimulation of heart rate.

Laerdal is a multinational company that develops products and programs for healthcare providers, voluntary organizations, educational institutions, hospitals, and the military worldwide. Laerdal has over 2,000 employees in 26 countries. The headquarters is located in Stavanger, Norway.

The University of Ottawa Heart Institute (UOHI) (French: Institut de cardiologie de l'Université d'Ottawa ) is Canada's largest cardiovascular health centre. It is located in Ottawa, Ontario, Canada. It began as a department in The Ottawa Hospital, and since has evolved into a complete cardiac centre, encompassing prevention, diagnosis, treatment, rehabilitation, research, and education.

Cardiac markers are biomarkers measured to evaluate heart function. They can be useful in the early prediction or diagnosis of disease. Although they are often discussed in the context of myocardial infarction, other conditions can lead to an elevation in cardiac marker level.
In health care, a simulated patient (SP), also known as a standardized patient, sample patient, or patient instructor, is an individual trained to act as a real patient in order to simulate a set of symptoms or problems. Simulated patients have been successfully utilized for education, evaluation of health care professionals, as well as basic, applied, and translational medical research.
The cardiac index (CI) is a hemodynamic measure that represents the cardiac output (CO) of an individual divided by their body surface area (BSA), expressed in liters per minute per square meter (L/min/m²). This parameter provides a more accurate assessment of heart function relative to the size of the individual, as opposed to absolute cardiac output alone. Cardiac index is crucial in assessing patients with heart failure and other cardiovascular conditions, providing insight into the adequacy of cardiac function in relation to the individual's metabolic needs.
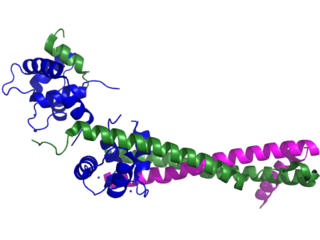
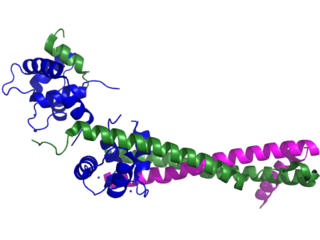
Troponin I is a cardiac and skeletal muscle protein family. It is a part of the troponin protein complex, where it binds to actin in thin myofilaments to hold the actin-tropomyosin complex in place. Troponin I prevents myosin from binding to actin in relaxed muscle. When calcium binds to the troponin C, it causes conformational changes which lead to dislocation of troponin I. Afterwards, tropomyosin leaves the binding site for myosin on actin leading to contraction of muscle. The letter I is given due to its inhibitory character. It is a useful marker in the laboratory diagnosis of heart attack. It occurs in different plasma concentration but the same circumstances as troponin T - either test can be performed for confirmation of cardiac muscle damage and laboratories usually offer one test or the other.

Myocardial perfusion imaging or scanning is a nuclear medicine procedure that illustrates the function of the heart muscle (myocardium).
Cardiac rehabilitation (CR) is defined by the World Health Organization (WHO) as "the sum of activity and interventions required to ensure the best possible physical, mental, and social conditions so that patients with chronic or post-acute cardiovascular disease may, by their own efforts, preserve or resume their proper place in society and lead an active life". CR is a comprehensive model of care delivering established core components, including structured exercise, patient education, psychosocial counselling, risk factor reduction and behaviour modification, with a goal of optimizing patient's quality of life and reducing the risk of future heart problems.

Redmond P. Burke is an American congenital heart surgeon, innovator, software developer, author, inventor, and founder of The Congenital Heart Institute at Miami Children's Hospital in Miami, Florida. He starred in the ABC pilot television show The Miracle Workers. Burke has been recognized as one of the world's most innovative surgeons, and for his use of information technology to improve surgical outcomes.
Computer-aided auscultation (CAA), or computerized assisted auscultation, is a digital form of auscultation. It includes the recording, visualization, storage, analysis and sharing of digital recordings of heart or lung sounds. The recordings are obtained using an electronic stethoscope or similarly suitable recording device. Computer-aided auscultation is designed to assist health care professionals who perform auscultation as part of their diagnostic process. Commercial CAA products are usually classified as clinical decision support systems that support medical professionals in making a diagnosis. As such they are medical devices and require certification or approval from a competent authority.
Neurocardiology is the study of the neurophysiological, neurological and neuroanatomical aspects of cardiology, including especially the neurological origins of cardiac disorders. The effects of stress on the heart are studied in terms of the heart's interactions with both the peripheral nervous system and the central nervous system.

MSR – The Israel Center for Medical Simulation is Israel's national institute for simulation-based medical education (SBME) and patient safety training. It is located at the Chaim Sheba Medical Center in the Tel HaShomer neighborhood of Ramat Gan, in the Tel Aviv District. MSR is internationally recognized as leader in patient safety simulation-based training.

Shelby Kutty is an Indian-born American cardiologist, a professor of pediatrics and internal medicine at the Johns Hopkins University School of Medicine. He holds the Helen B. Taussig endowed professorship at Johns Hopkins and is Director of the Helen B. Taussig Heart Center and the chair of Cardiovascular Analytic Intelligence Initiative at Johns Hopkins Hospital. He currently serves as the editor of American Journal of Physiology: Heart and Circulatory Physiology and Cardiology in the Young and as consulting editor for the Journal of Clinical Investigation. Prior to this, he held the title of assistant dean for research and development and vice chair of pediatrics at the University of Nebraska Medical Center College of Medicine. Kutty has published over 400 articles in peer-reviewed medical journals.

Mark Edwin Silverman MD MACP FACC was an American cardiologist, medical historian, medical educator and author of more than 200 medical articles and a number of books, who founded the cardiology program at Piedmont Hospital in Atlanta, Georgia.

Jason C. Kovacic is an Australian-born cardiologist and physician-scientist; the Robert Graham Chair and Professor of Medicine, University of New South Wales; Executive Director of the Victor Chang Cardiac Research Institute in Sydney, Australia; and Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai, New York.
Harvey Feigenbaum is an American cardiologist known for his life-long work in the field of echocardiography. He wrote the first textbook on the subject in 1972, which is currently in its 8th edition, and has published over 300 articles. He has trained generations of cardiologists including many of the world's pioneers in the field through his numerous visitors, frequent workshops, annual courses in Indianapolis, Indiana beginning in 1968, the year when he started formal fellowship training He founded the field of cardiac sonography in 1965 and the American Society of Echocardiography in 1975. His seminal article on the diagnosis of pericardial effusions published in 1965 with his technique "brought echocardiography to the attention of thousands of practitioners".