Weston General Hospital is an NHS district general hospital in the town of Weston-super-Mare, Somerset, England, operated by University Hospitals Bristol and Weston NHS Foundation Trust. As of June 2019, the hospital had 261 beds and around 1,800 clinical and non-clinical staff. It has a part-time Accident & Emergency department, an intensive care unit, an oncology and haematology day unit, and a day case unit. The hospital also has a 12-bed private unit, The Waterside Suite, wholly owned by the hospital trust, with profits being re-invested into the main hospital.
A virtual ward allows patients to get the care they need at home safely and conveniently, rather than being in hospital.

BMI Healthcare was an independent provider of private healthcare, offering treatment to private patients, medically insured patients, and NHS patients. As of 2019, it had 54 private hospitals and healthcare facilities across the UK, with headquarters in London. In December 2019, it was acquired by a parent company of Circle Health and was replaced by Circle Health Group in 2022.

Clinical commissioning groups (CCGs) were National Health Service (NHS) organisations set up by the Health and Social Care Act 2012 to organise the delivery of NHS services in each of their local areas in England. On 1 July 2022 they were abolished, and replaced by Integrated care systems as a result of the Health and Care Act 2022.

NHS England, officially the NHS Commissioning Board, is an executive non-departmental public body of the Department of Health and Social Care. It oversees the budget, planning, delivery and day-to-day operation of the commissioning side of the National Health Service in England as set out in the Health and Social Care Act 2012. It directly commissions NHS general practitioners, dentists, optometrists and some specialist services. The Secretary of State publishes annually a document known as the NHS mandate which specifies the objectives which the Board should seek to achieve. National Health Service Regulations are published each year to give legal force to the mandate.
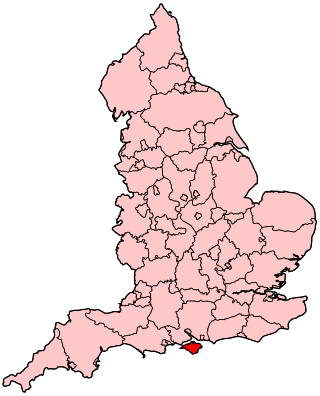
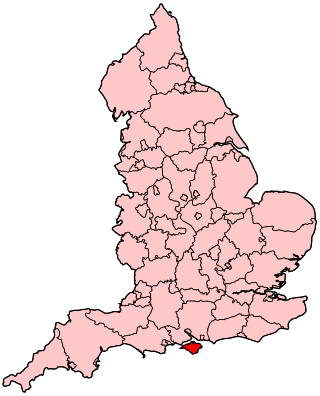
The Isle of Wight NHS Trust is an NHS trust which provides physical health, mental health and ambulance services for the Isle of Wight. The trust is unique in being the only integrated acute, community, mental health and ambulance health care provider in England. It runs St Mary's Hospital and the Isle of Wight Ambulance Service.
The Medical Technology Group (MTG) is a not for profit organisation in the United Kingdom comprising patient groups, research charities and medical device manufacturers. Its stated aim is to "work together to improve patient access to effective medical technologies". The Group launched in 2001.
Healthcare in London, which consumes about a fifth of the NHS budget in England, is in many respects distinct from that in the rest of the United Kingdom, or England.
Healthcare in Dorset was primarily the responsibility of Dorset Clinical Commissioning Group until July 2022. Dorset County Council is leading in the development of an electronic health record, to be called the Dorset Care Record, provided by Orion Health. It is intended to enable all health and social care providers to share records.

Healthcare in Kent has, from 1 July 2022, been mainly the responsibility of the Kent & Medway Integrated Care Board. Certain specialised services are directly commissioned by NHS England, coordinated through the South East integrated regional team. Some NHS England structures are aligned on a Kent and Medway basis, others on a South East basis and there is liaison with London to provide many tertiary healthcare services.
Healthcare in Somerset, England was the responsibility of three clinical commissioning groups (CCGs) until July 2022. These covered the ceremonial county of Somerset, which comprises the areas governed by the three unitary authorities of Somerset, North Somerset and Bath and North East Somerset.
The "Greater Manchester Model" of NHS health care was a system uniquely devolved within England, by way of close integration with the Greater Manchester Combined Authority and local authorities, led by the Mayor of Greater Manchester. In July 2022 the Greater Manchester integrated care system took over responsibility for health and social care in the conurbation. The financial plan for 2022–23 had an initial shortage of £187 million.
Healthcare in the West Midlands was, until July 2022, the responsibility of five integrated care groups: Birmingham and Solihull, Sandwell and West Birmingham, Dudley, Wolverhampton, and Walsall.
Healthcare in Essex is now the responsibility of six clinical commissioning groups: Basildon and Brentwood, Mid Essex, North East Essex, Southend, Thurrock and West Essex.
Healthcare in Gloucestershire was the responsibility of two clinical commissioning groups, covering Gloucestershire and South Gloucestershire, until July 2022. The health economy of Gloucestershire has always been linked with that of Bristol.
Healthcare in Hampshire was the responsibility of six clinical commissioning groups until July 2022. These were based in Southampton, Portsmouth, North East Hampshire and Farnham, South Eastern Hampshire, West Hampshire, and North Hampshire. In 2018, the Hampshire and Isle of Wight Partnership of Clinical Commissioning Groups was set up. Maggie MacIsaac was Chief Executive.
Healthcare in Lancashire in 2015 was the responsibility of seven clinical commissioning groups covering Blackpool, Chorley and South Ribble, East Lancashire, Fylde and Wyre, Greater Preston, Lancaster North and West Lancashire. In 1 April 2017 32 GP practices from Cumbria Clinical Commissioning Group merged with Lancashire North CCG to form Morecambe Bay CCG which was abolished in July 2022 when integrated care systems were introduced.
Healthcare in Yorkshire from 2016 was the responsibility of 19 clinical commissioning groups, which were replaced by integrated care systems in July 2022.
Healthcare in Cheshire was the responsibility of Eastern Cheshire, South Cheshire, Vale Royal and West Cheshire clinical commissioning groups until July 2022.
Healthcare in Buckinghamshire was the responsibility for the Aylesbury Vale, Chiltern, and Milton Keynes. clinical commissioning groups until July 2022.