Related Research Articles

Tokelau is a dependent territory of New Zealand in the southern Pacific Ocean. It consists of three tropical coral atolls, with a combined land area of 10 km2 (4 sq mi). The capital rotates yearly among the three atolls. Tokelau lies north of the Samoan Islands, east of Tuvalu, south of the Phoenix Islands, southwest of the more distant Line Islands, and northwest of the Cook Islands. Swains Island is subject to an ongoing territorial dispute and is currently administered by the United States as part of American Samoa.
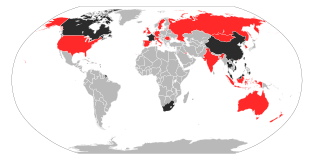
The 2002–2004 SARS outbreak was an epidemic involving severe acute respiratory syndrome (SARS) caused by severe acute respiratory syndrome coronavirus. The outbreak was first identified in Foshan, Guangdong, China, in November 16, 2002.
This article contains links to Lists of hospitals in the United States, including U.S. States, the District, insular areas, and outlying islands. Links to more detailed state lists are shown. According to a report by the Sheps Center for Health Services Research at the University of North Carolina in 2017, 79 mostly rural hospitals have closed since 2010, mostly across the Southern United States.

This is a list of hospitals in Oceania for each sovereign state, associated states of New Zealand, and dependencies, and territories. Links to lists of hospitals in countries are used when there are more than a few hospitals in the country. Oceania has an area of 8,525,989 km2 and population of 41,570,842 (2018). The World Health Organization surveys of healthcare in smaller countries are used to identify hospitals in smaller countries.

The politics of Tokelau takes place within a framework of a parliamentary representative democratic dependency. The head of state of Tokelau is Queen Elizabeth II in right of her Realm of New Zealand, who is represented by an Administrator. The monarch is hereditary, the Administrator is appointed by the New Zealand Minister of Foreign Affairs and Trade.
Algeria is the largest country in Africa and is estimated to have a population of around 40 million people. Algeria has a public health care system, which is accessible and free of charge to all citizens of Algeria. The public health care system is financed by the government of Algeria. Given Algeria's young population, policy favors preventive health care and clinics over hospitals. In keeping with this policy, the government maintains an intensive immunization programme and a policy which allows Algerian citizens health care for Hospitalisations, medicines and outpatient care free to all citizens of Algeria.

Healthcare in China consists of both public and private medical institutions and insurance programs. About 95% of the population has at least basic health insurance coverage. Despite this, public health insurance generally only covers about half of medical costs, with the proportion lower for serious or chronic illnesses. Under the "Healthy China 2020" initiative, China is currently undertaking an effort to cut healthcare costs, and the government requires that insurance will cover 70% of costs by the end of 2018. The Chinese government is working on providing affordable basic healthcare to all residents by 2020. China has also become a major market for health-related multinational companies. Companies such as AstraZeneca, GlaxoSmithKline, Eli Lilly, and Merck entered the Chinese market and have experienced explosive growth. China has also become a growing hub for healthcare research and development. According to Sam Radwan of ENHANCE International, China’s projected healthcare spending in 2050 may exceed Germany’s entire 2020 gross domestic product.

The National Health Service (NHS) is the publicly funded healthcare system in England, and one of the four National Health Service systems in the United Kingdom. It is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde. Primarily funded by the government from general taxation, and overseen by the Department of Health and Social Care, the NHS provides healthcare to all legal English residents and residents from other regions of the UK, with most services free at the point of use. Some services, such as emergency treatment and treatment of infectious diseases, are free for everyone, including visitors.

The National Health Service (NHS) is the publicly-funded healthcare system of the United Kingdom. Since 1948 it has been funded out of general taxation. It is made up of four separate systems that serve each part of the UK: The National Health Service in England, NHS Scotland, NHS Wales, and Health and Social Care in Northern Ireland. They were established together in 1948 as one of the major social reforms following the Second World War. The founding principles were that services should be comprehensive, universal and free at the point of delivery. Each service provides a comprehensive range of health services, free at the point of use for people ordinarily resident in the United Kingdom, apart from dental treatment and optical care. In England, NHS patients have to pay prescription charges with a range of exemptions from these charges.
Health care in the United States is provided by many distinct organizations. Health care facilities are largely owned and operated by private sector businesses. 58% of community hospitals in the United States are non-profit, 21% are government-owned, and 21% are for-profit. According to the World Health Organization (WHO), the United States spent $9,403 on health care per capita, and 17.1% on health care as percentage of its GDP in 2014. Healthcare coverage is provided through a combination of private health insurance and public health coverage. The United States does not have a universal healthcare program, unlike most other developed countries.

North Korea has a life expectancy of 71.69 years as of 2016. While North Korea is classified as a low-income country, the structure of North Korea's causes of death (2013) is unlike that of other low-income countries. Instead, it is closer to the worldwide averages, with non-communicable diseases – such as cardiovascular disease – accounting for two-thirds of the total deaths.

In Norway, all hospitals are funded by the public as part of the national budget. However, while medical treatment is free of charge for any person younger than the age of sixteen, residents who have reached adulthood must pay a deductible each year before becoming eligible for an exemption card. The card entitles one to free healthcare for the remainder of that year.
Princess Margaret Hospital (PMH) on Funafuti atoll in Tuvalu is the only hospital in the country, and the primary provider of medical services for all the islands of Tuvalu. The hospital is located about 1.3 kilometres north from the centre of Funafuti on Fongafale islet.
As prescribed in the Constitution of Tokelau, individual human rights are those found in the Universal Declaration of Human Rights and reflected in the International Covenant on Civil and Political Rights. When exercising these rights, there must be proper recognition of the rights of others and to the community as a whole. If an individual believes their rights have been breached they may go to the Council for the Ongoing Government who may make any appropriate order to protect that individual’s rights. There have been no such complaints to date.

The ongoing pandemic of coronavirus disease 2019, a novel infectious disease caused by severe acute respiratory syndrome coronavirus 2, spread to the Philippines on January 30, 2020, when the first case was confirmed in Metro Manila. It involved a 38-year-old Chinese woman who was confined in the San Lazaro Hospital in Manila. The second case was confirmed on February 2, that of a 44-year-old Chinese man who died a day earlier, which was also the first confirmed death from the disease outside mainland China. The first case of someone without travel history abroad was confirmed on March 5, a 62-year-old male who frequented a Muslim prayer hall in San Juan, Metro Manila, raising suspicions that a community transmission of COVID-19 is already underway in the Philippines. The man's wife was confirmed to have contracted COVID-19 on March 7, which was also the first local transmission to be confirmed.

2020 coronavirus pandemic is an ongoing pandemic of coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first case was officially confirmed in Slovenia on 4 March 2020. It was imported case from by a tourist traveling from Morocco via Italy, which is the center of the SARS-CoV-2 in Europe. First days of the pandemic were challenging for Slovenia due to the resignation of Prime Minister Marjan Šarec in late January and the consequent formation of new government. First case was confirmed one day after Janez Janša was elected Prime Minister. During the transition period, the outbreak escalated. A joint meeting between the outgoing and incoming government was held on 10 March 2020. Outgoing caretaker government of Marjan Šarec was responsible for the crisis management until 14 March 2020.
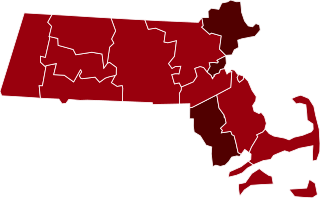
The 2020 coronavirus pandemic in Massachusetts is part of an ongoing pandemic of coronavirus disease 2019 (COVID-19) in the U.S. state of Massachusetts. The first confirmed case was reported on February 1, 2020, and the number of cases began increasing rapidly on March 5. Governor Charlie Baker declared a state of emergency on March 10. By March 12, over 100 people had tested positive for the virus. Most early cases were traceable to a company meeting held in Boston in late February by the Cambridge-based biotechnology firm Biogen. Massachusetts is third in the U.S. for overall number of cases statewide. As of April 29, 2020, there were 60,265 confirmed cases and 3,405 deaths due to COVID-19. Massachusetts had performed 265,618 tests, 22.7% of which were positive.
Ai Fen is a Chinese doctor and director of the emergency department of Central Hospital of Wuhan. She is the first medical personnel to disclose the 2019–20 coronavirus epidemic to the outside world. She was given the nickname "The Whistle-Giver" (发哨子的人) in an article in the Chinese Renwu magazine, which the Chinese government censored, but which was reposted on the Chinese internet using emojis, Morse code and pinyin to circumvent censorship.
The 2020 coronavirus pandemic in Ontario is an ongoing viral pandemic of coronavirus disease 2019 (COVID-19), a novel infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first identified case of COVID-19 in Canada during the 2019–20 worldwide pandemic occurred in the Canadian province of Ontario after it arrived on January 22, 2020, when a man returned to Toronto from travel in China, including Wuhan; the case was announced on January 25. The government announced on March 17 that Ontario had "some evidence of community transmission" of COVID-19.

A health care desert, strictly defined, is a populated area more than 60 miles drive from an acute-care hospital offering emergency room services. An estimated 30 million Americans, many in rural regions of the country, live at least 60 minutes drive from a hospital with trauma care services. Limited access to emergency room services, as well as medical specialists, leads to increases in mortality rates and long-term health problems, such as heart disease and diabetes. Regions with higher rates of Medicaid and Medicare patients, as well patients who are uninsured are less likely to live within an hour's drive of a hospital emergency room. Since 1975, over 1,000 hospitals, many in rural regions, have closed their doors, unable to bear the cost of care of uninsured patients, resulting in some patients in every state needing to drive at least an hour to a hospital emergency room, a problem that poses an even greater danger during the COVID-19 pandemic, when patients in respiratory distress urgently need oxygenand can ill afford an hour-long ambulance ride to reach a hospital.
References
- 1 2 3 "Tokelau NCD Risk factors" (PDF). WHO. Retrieved April 28, 2020.
- 1 2 "Tokelau, Department of Health". Tokelau.org. Retrieved April 28, 2020.
- ↑ "About Tokelau". Tokelau.org.naz. Retrieved April 28, 2020.