Nauru, officially the Republic of Nauru and formerly known as Pleasant Island, is an island country and microstate in Micronesia, part of Oceania in the Central Pacific. Its nearest neighbour is Banaba of Kiribati, about 300 km (190 mi) to the east. It lies northwest of Tuvalu, 1,300 km (810 mi) northeast of Solomon Islands, east-northeast of Papua New Guinea, southeast of the Federated States of Micronesia and south of the Marshall Islands. With an area of only 21 km2 (8.1 sq mi), Nauru is the third-smallest country in the world behind Vatican City and Monaco, making it the smallest republic and island nation. Its population of about 10,800 is the world's second-smallest after Vatican City. Settled by people from Micronesia circa 1000 BCE, Nauru was annexed and claimed as a colony by the German Empire in the late 19th century. After World War I, Nauru became a League of Nations mandate administered by Australia, New Zealand, and the United Kingdom. During World War II, Nauru was occupied by Japanese troops, and was bypassed by the Allied advance across the Pacific. After the war ended, the country entered into United Nations trusteeship. Nauru gained its independence in 1968.

The demographics of Nauru, an island country in the Pacific Ocean, are known through national censuses, which have been analysed by various statistical bureaus since the 1920s. The Nauru Bureau of Statistics have conducted this task since 1977—the first census since Nauru gained independence in 1968. The most recent census of Nauru was in 2011, when population had reached ten thousand. The population density is 478 inhabitants per square kilometre, and the overall life expectancy is 59.7 years. The population rose steadily from the 1960s until 2006 when the Government of Nauru repatriated thousands of Tuvaluan and I-Kiribati workers from the country. Since 1992, Nauru's birth rate has exceeded its death rate; the natural growth rate is positive. In terms of age structure, the population is dominated by the 15–64-year-old segment (65.6%). The median age of the population is 21.5, and the estimated gender ratio of the population is 0.91 males per one female.

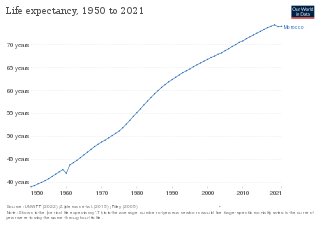
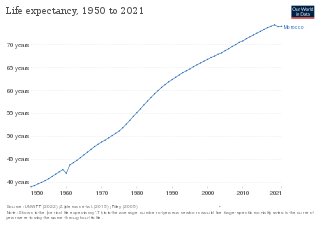
Health in Uganda refers to the health of the population of Uganda. The average life expectancy at birth of Uganda has increased from 59.9 years in 2013 to 63.4 years in 2019. This is lower than in any other country in the East African Community except Burundi. As of 2017, females had a life expectancy higher than their male counterparts of 69.2 versus 62.3. It is projected that by 2100, males in Uganda will have an expectancy of 74.5 and females 83.3. Uganda's population has steadily increased from 36.56 million in 2016 to an estimate of 42.46 in 2021. The fertility rate of Ugandan women slightly increased from an average of 6.89 babies per woman in the 1950s to about 7.12 in the 1970s before declining to an estimate 5.32 babies in 2019. This figure is higher than most world regions including South East Asia, Middle East and North Africa, Europe and Central Asia and America. The under-5-mortality-rate for Uganda has decreased from 191 deaths per 1000 live births in 1970 to 45.8 deaths per 1000 live births in 2019.

Pakistan is the fifth most populous country in the world with population approaching 225 million. It is a developing country struggling in many domains due to which the health system has suffered a lot. As a result of that, Pakistan is ranked 122nd out of 190 countries in the World Health Organization performance report.
Australia is a high income country, and this is reflected in the good status of health of the population overall. In 2011, Australia ranked 2nd on the United Nations Development Programme's Human Development Index, indicating the level of development of a country. Despite the overall good status of health, the disparities occurring in the Australian healthcare system are a problem. The poor and those living in remote areas as well as indigenous people are, in general, less healthy than others in the population, and programs have been implemented to decrease this gap. These include increased outreach to the indigenous communities and government subsidies to provide services for people in remote or rural areas.

Mali, one of the world's poorest nations, is greatly affected by poverty, malnutrition, epidemics, and inadequate hygiene and sanitation. Mali's health and development indicators rank among the worst in the world, with little improvement over the last 20 years. Progress is impeded by Mali's poverty and by a lack of physicians. The 2012 conflict in northern Mali exacerbated difficulties in delivering health services to refugees living in the north.
Morocco became an independent country in 1956. At that time there were only 400 private practitioners and 300 public health physicians in the entire country. By 1992, the government had thoroughly improved their health care service and quality. Health care was made available to over 70% of the population. Programs and courses to teach health and hygiene have been introduced to inform parents and children on how to correctly care for their own and their families' health.
Sudan is still one of the largest countries in Africa even after the split of the Northern and Southern parts. It is one of the most densely populated countries in the region and is home to over 37.9 million people.

Healthcare in Turkey consists of a mix of public and private health services. Turkey introduced universal health care in 2003. Known as Universal Health Insurance Genel Sağlık Sigortası, it is funded by a tax surcharge on employers, currently at 5%. Public-sector funding covers approximately 75.2% of health expenditures.
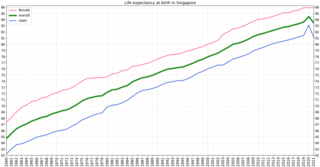
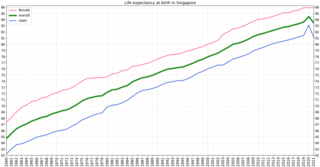
Singapore is one of the wealthiest countries in the world, with a gross domestic product (GDP) per capita of more than $57,000. Life expectancy at birth is 82.3 and infant mortality is 2.7 per 1000 live births. The population is ageing and by 2030, 20% will be over 65. However it is estimated that about 85% of those over 65 are healthy and reasonably active. Singapore has a universal health care system.

The major causes of deaths in Finland are cardiovascular diseases, malignant tumors, dementia and Alzheimer's disease, respiratory diseases, alcohol related diseases and accidental poisoning by alcohol. In 2010 the leading causes of death among men aged 15 to 64 were alcohol related deaths, ischaemic heart disease, accident, suicides, lung cancer and cerbrovascular diseases. Among women the leading causes were breast cancer, alcohol related deaths, accidents, suicides, ischaemic heart disease and lung cancer.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).
Botswana's healthcare system has been steadily improving and expanding its infrastructure to become more accessible. The country's position as an upper middle-income country has allowed them to make strides in universal healthcare access for much of Botswana's population. The majority of the Botswana's 2.3 million inhabitants now live within five kilometers of a healthcare facility. As a result, the infant mortality and maternal mortality rates have been on a steady decline. The country's improving healthcare infrastructure has also been reflected in an increase of the average life expectancy from birth, with nearly all births occurring in healthcare facilities.

Health in Chad is suffering due to the country's weak healthcare system. Access to medical services is very limited and the health system struggles with shortage of medical staff, medicines and equipment. In 2018, the UNHCR reported that Chad currently has 615,681 people of concern, including 446,091 refugees and asylum seekers. There is a physician density of 0.04 per 1,000 population and nurse and midwife density of 0.31 per 1,000 population. The life expectancy at birth for people born in Chad, is 53 years for men and 55 years for women (2016). In 2019 Chad ranked as 187 out of 189 countries on the human development index, which places the country as a low human development country.
The fertility rate was approximately 3.7 per woman in Honduras in 2009. The under-five mortality rate is at 40 per 1,000 live births. The health expenditure was US$197 per person in 2004. There are about 57 physicians per 100,000 people.

New Zealand is a high income country, and this is reflected in the overall good health status of the population. However like other wealthy countries, New Zealand suffers from high rates of obesity and heart disease.

Brunei's healthcare system is managed by the Brunei Ministry of Health and funded by the General Treasury. It consists of around 15 health centers, ten clinics and 22 maternal facilities, considered to be of reasonable standard. There are also two private hospitals. Cardiovascular disease, cancer, and diabetes are the leading cause of death in the country, with life expectancy around 75 years, a vast improvement from 1961. Brunei's human development index (HCI) improved from 0.81 in 2002 to 0.83 in 2021, expanding at an average annual rate of 0.14%. According to the UN's Human Development Report 2020, the HCI for girls in the country is greater than for boys, though aren't enough statistics in Brunei to break down HCI by socioeconomic classes. Brunei is the second country in Southeast Asia after Singapore to be rated 47th out of 189 nations on the UN HDI 2019 and has maintained its position in the Very High Human Development category. Being a culturally taboo subject, the rate of suicide has not been investigated.
Health indicators are quantifiable characteristics of a population which researchers use as supporting evidence for describing the health of a population. Typically, researchers will use a survey methodology to gather information about a population sample, use statistics in an attempt to generalize the information collected to the entire population, and then use the statistical analysis to make a statement about the health of the population. Health indicators are often used by governments to guide health care policy or to make goals for improving population health.
This article summarizes healthcare in Texas. In 2022, the United Healthcare Foundation ranked Texas as the 38th healthiest state in the United States. Obesity, excessive drinking, maternal mortality, infant mortality, vaccinations, mental health, and limited access to healthcare are among the major public health issues facing Texas.
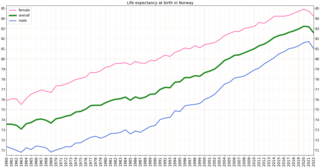
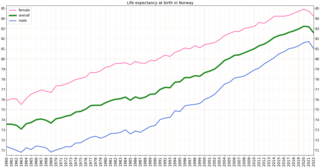
Health in Norway, with its early history of poverty and infectious diseases along with famines and epidemics, was poor for most of the population at least into the 1800s. The country eventually changed from a peasant society to an industrial one and established a public health system in 1860. Due to the high life expectancy at birth, the low under five mortality rate and the fertility rate in Norway, it is fair to say that the overall health status in the country is generally good.