Related Research Articles

Tumor hypoxia is the situation where tumor cells have been deprived of oxygen. As a tumor grows, it rapidly outgrows its blood supply, leaving portions of the tumor with regions where the oxygen concentration is significantly lower than in healthy tissues. Hypoxic microenvironments in solid tumors are a result of available oxygen being consumed within 70 to 150 μm of tumor vasculature by rapidly proliferating tumor cells thus limiting the amount of oxygen available to diffuse further into the tumor tissue. In order to support continuous growth and proliferation in challenging hypoxic environments, cancer cells are found to alter their metabolism. Furthermore, hypoxia is known to change cell behavior and is associated with extracellular matrix remodeling and increased migratory and metastatic behavior.
The epithelial–mesenchymal transition (EMT) is a process by which epithelial cells lose their cell polarity and cell–cell adhesion, and gain migratory and invasive properties to become mesenchymal stem cells; these are multipotent stromal cells that can differentiate into a variety of cell types. EMT is essential for numerous developmental processes including mesoderm formation and neural tube formation. EMT has also been shown to occur in wound healing, in organ fibrosis and in the initiation of metastasis in cancer progression.

Targeted therapy or molecularly targeted therapy is one of the major modalities of medical treatment (pharmacotherapy) for cancer, others being hormonal therapy and cytotoxic chemotherapy. As a form of molecular medicine, targeted therapy blocks the growth of cancer cells by interfering with specific targeted molecules needed for carcinogenesis and tumor growth, rather than by simply interfering with all rapidly dividing cells. Because most agents for targeted therapy are biopharmaceuticals, the term biologic therapy is sometimes synonymous with targeted therapy when used in the context of cancer therapy. However, the modalities can be combined; antibody-drug conjugates combine biologic and cytotoxic mechanisms into one targeted therapy.
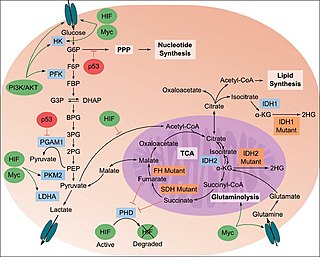
The study of the tumor metabolism, also known as tumor metabolome describes the different characteristic metabolic changes in tumor cells. The characteristic attributes of the tumor metabolome are high glycolytic enzyme activities, the expression of the pyruvate kinase isoenzyme type M2, increased channeling of glucose carbons into synthetic processes, such as nucleic acid, amino acid and phospholipid synthesis, a high rate of pyrimidine and purine de novo synthesis, a low ratio of Adenosine triphosphate and Guanosine triphosphate to Cytidine triphosphate and Uridine triphosphate, low Adenosine monophosphate levels, high glutaminolytic capacities, release of immunosuppressive substances and dependency on methionine.

The Von Hippel–Lindau tumor suppressor also known as pVHL is a protein that, in humans, is encoded by the VHL gene. Mutations of the VHL gene are associated with Von Hippel–Lindau disease, which is characterized by hemangioblastomas of the brain, spinal cord and retina. It is also associated with kidney and pancreatic lesions.
Triple-negative breast cancer (TNBC) is any breast cancer that either lacks or shows low levels of estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (HER2) overexpression and/or gene amplification. Triple-negative is sometimes used as a surrogate term for basal-like.

Metastasis-associated protein MTA1 is a protein that in humans is encoded by the MTA1 gene. MTA1 is the founding member of the MTA family of genes. MTA1 is primarily localized in the nucleus but also found to be distributed in the extra-nuclear compartments. MTA1 is a component of several chromatin remodeling complexes including the nucleosome remodeling and deacetylation complex (NuRD). MTA1 regulates gene expression by functioning as a coregulator to integrate DNA-interacting factors to gene activity. MTA1 participates in physiological functions in the normal and cancer cells. MTA1 is one of the most upregulated proteins in human cancer and associates with cancer progression, aggressive phenotypes, and poor prognosis of cancer patients.

Metastasis-associated protein MTA3 is a protein that in humans is encoded by the MTA3 gene. MTA3 protein localizes in the nucleus as well as in other cellular compartments MTA3 is a component of the nucleosome remodeling and deacetylate (NuRD) complex and participates in gene expression. The expression pattern of MTA3 is opposite to that of MTA1 and MTA2 during mammary gland tumorigenesis. However, MTA3 is also overexpressed in a variety of human cancers.

Epithelioid sarcoma is a rare soft tissue sarcoma arising from mesenchymal tissue and characterized by epithelioid-like features. It accounts for less than 1% of all soft tissue sarcomas. It was first definitively characterized by F.M. Enzinger in 1970. It commonly presents itself in the distal limbs of young adults as a small, soft mass or a cluster of bumps. A proximal version has also been described, frequently occurring in the upper extremities. Less commonly, cases are reported in the pelvis, vulva, penis, and spine.

Evofosfamide is a compound being evaluated in clinical trials for the treatment of multiple tumor types as a monotherapy and in combination with chemotherapeutic agents and other targeted cancer drugs.
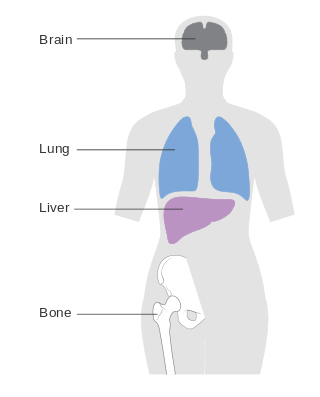
Metastatic breast cancer, also referred to as metastases, advanced breast cancer, secondary tumors, secondaries or stage IV breast cancer, is a stage of breast cancer where the breast cancer cells have spread to distant sites beyond the axillary lymph nodes. There is no cure for metastatic breast cancer; there is no stage after IV.

A brain metastasis is a cancer that has metastasized (spread) to the brain from another location in the body and is therefore considered a secondary brain tumor. The metastasis typically shares a cancer cell type with the original site of the cancer. Metastasis is the most common cause of brain cancer, as primary tumors that originate in the brain are less common. The most common sites of primary cancer which metastasize to the brain are lung, breast, colon, kidney, and skin cancer. Brain metastases can occur months or even years after the original or primary cancer is treated. Brain metastases have a poor prognosis for cure, but modern treatments allow patients to live months and sometimes years after the diagnosis.
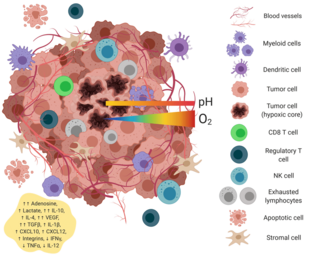
The tumor microenvironment is a complex ecosystem surrounding a tumor, composed of cancer cells, stromal tissue and the extracellular matrix. Mutual interaction between cancer cells and the different components of the tumor microenvironment support its growth and invasion in healthy tissues which correlates with tumor resistance to current treatments and poor prognosis. The tumor microenvironment is in constant change because of the tumor's ability to influence the microenvironment by releasing extracellular signals, promoting tumor angiogenesis and inducing peripheral immune tolerance, while the immune cells in the microenvironment can affect the growth and evolution of cancerous cells.
Directed enzyme prodrug therapy (DEPT) uses enzymes artificially introduced into the body to convert prodrugs, which have no or poor biologically activity, to the active form in the desired location within the body. Many chemotherapy drugs for cancer lack tumour specificity and the doses required to reach therapeutic levels in the tumour are often toxic to other tissues. DEPT strategies are an experimental method of reducing the systemic toxicity of a drug, by achieving high levels of the active drug only at the desired site. This article describes the variations of DEPT technology.

Vasculogenic mimicry (VM) is a strategy used by tumors to ensure sufficient blood supply is brought to its cells through establishing new tumor vascularization. This process is similar to tumor angiogenesis; on the other hand vascular mimicry is unique in that this process occurs independent of endothelial cells. Vasculature is instead developed de novo by cancer cells, which under stress conditions such as hypoxia, express similar properties to stem cells, capable of differentiating to mimic the function of endothelial cells and form vasculature-like structures. The ability of tumors to develop and harness nearby vasculature is considered one of the hallmarks of cancer disease development and is thought to be closely linked to tumor invasion and metastasis. Vascular mimicry has been observed predominantly in aggressive and metastatic cancers and has been associated with negative tumor characteristics such as increased metastasis, increased tissue invasion, and overall poor outcomes for patient survival. Vascular mimicry poses a serious problem for current therapeutic strategies due to its ability to function in the presence of Anti-angiogenic therapeutic agents. In fact, such therapeutics have been found to actually drive VM formation in tumors, causing more aggressive and difficult to treat tumors to develop.
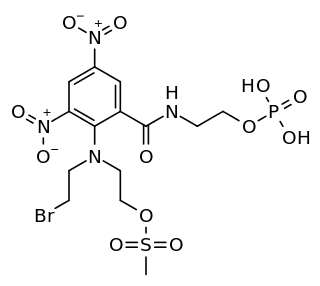
PR-104 is a drug from the class of hypoxia-activated prodrugs (HAPs), which is being researched as a potential anti-cancer therapeutic agent. It is a phosphate ester “pre-prodrug” that is rapidly converted to the HAP PR-104A in the body. PR-104A is in turn metabolised to reactive nitrogen mustard DNA crosslinking agents in hypoxic tissues such as found in solid tumours. Following initial clinical studies, it was discovered that PR-104A is also activated by the enzyme AKR1C3, independently of hypoxia. Hypoxia in the bone marrow of patients with leukaemia, and high activity of AKR1C3 in some leukaemia subtypes has led to interest in clinical trials of PR-104 in relapsed refractory acute leukaemias.
A pre-metastatic niche is an environment in a secondary organ that can be conducive to the metastasis of a primary tumor. Such a niche provides favorable conditions for growth, and eventual metastasis, in an otherwise foreign and hostile environment for the primary tumor cells. This concept demonstrated the fundamental role of the microenvironment in regulating tumor growth and metastasis. The discovery of the pre-metastatic niche has fostered new research regarding the potential treatment of metastases, including targeting myeloid derived suppressor cells, and stromal cell plasticity including fibroblasts and pericytes and perivascular smooth muscle cells and (attempts to stop the flow of vesicles from primary tumors to pre-metastatic niches in secondary organs and different combinations of microenvironment targeted therapies.
The host response to cancer therapy is defined as a physiological response of the non-malignant cells of the body to a specific cancer therapy. The response is therapy-specific, occurring independently of cancer type or stage.

Lurbinectedin, sold under the brand name Zepzelca, is a medication used for the treatment of small cell lung cancer.
pH-responsive tumor-targeted drug delivery is a specialized form of targeted drug delivery that utilizes nanoparticles to deliver therapeutic drugs directly to cancerous tumor tissue while minimizing its interaction with healthy tissue. Scientists have used drug delivery as a way to modify the pharmacokinetics and targeted action of a drug by combining it with various excipients, drug carriers, and medical devices. These drug delivery systems have been created to react to the pH environment of diseased or cancerous tissues, triggering structural and chemical changes within the drug delivery system. This form of targeted drug delivery is to localize drug delivery, prolongs the drug's effect, and protect the drug from being broken down or eliminated by the body before it reaches the tumor.
References
- ↑ Minchinton, Andrew I.; Tannock, Ian F. (August 2006). "Drug penetration in solid tumours". Nature Reviews Cancer. 6 (8): 583–592. doi:10.1038/nrc1893. PMID 16862189. S2CID 42818461.
- ↑ Gillies, Robert J.; Gatenby, Robert A. (3 April 2007). "Hypoxia and adaptive landscapes in the evolution of carcinogenesis". Cancer and Metastasis Reviews. 26 (2): 311–317. doi:10.1007/s10555-007-9065-z. PMID 17404691. S2CID 2276912.
- ↑ Sullivan, Richard; Graham, Charles H. (26 April 2007). "Hypoxia-driven selection of the metastatic phenotype". Cancer and Metastasis Reviews. 26 (2): 319–331. doi:10.1007/s10555-007-9062-2. PMID 17458507. S2CID 13457619.
- ↑ "Novacea to be acquired by Transcept Pharmaceuticals". Reuters. 2008-09-02. Retrieved 2016-03-22.
- ↑ "Paratek Pharmaceuticals Completes Merger With Transcept Pharmaceuticals". GlobeNewswire News Room (Press release). 30 October 2014. Retrieved 2016-03-22.
- ↑ "Convert Pharmaceuticals Home". Convert Pharmaceuticals. Retrieved 2025-01-26.
- ↑ "Our science: Hypoxia-Activated Prodrugs". Convert Pharmaceuticals. Retrieved 2025-01-26.
- ↑ "Tarloxotinib bromide* (TH-4000): Combining molecular targeting and hypoxia targeting in a single drug candidate". Threshold Pharmaceuticals. Archived from the original on 5 April 2016. Retrieved 24 March 2016.
- ↑ "Threshold Pharmaceuticals and Molecular Templates agree to combine". Reuters. March 17, 2017.