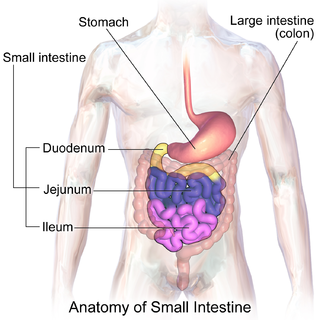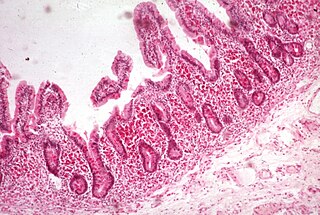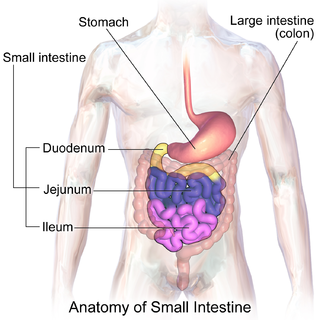
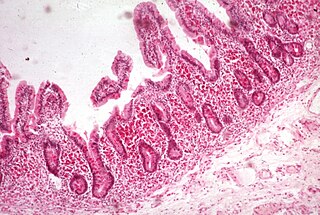
The small intestine or small bowel is an organ in the gastrointestinal tract where most of the absorption of nutrients from food takes place. It lies between the stomach and large intestine, and receives bile and pancreatic juice through the pancreatic duct to aid in digestion. The small intestine is about 5.5 metres long and folds many times to fit in the abdomen. Although it is longer than the large intestine, it is called the small intestine because it is narrower in diameter.

Gastric bypass surgery refers to a technique in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass procedures (GBP). Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.
A gastrectomy is a partial or total surgical removal of the stomach.
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal (GI) tract. Impairment can be of single or multiple nutrients depending on the abnormality. This may lead to malnutrition and a variety of anaemias.

Small intestinal bacterial overgrowth (SIBO), also termed bacterial overgrowth, or small bowel bacterial overgrowth syndrome (SBBOS), is a disorder of excessive bacterial growth in the small intestine. Unlike the colon, which is rich with bacteria, the small bowel usually has fewer than 100,000 organisms per millilitre. Patients with bacterial overgrowth typically develop symptoms which may include nausea, bloating, vomiting, diarrhea, malnutrition, weight loss and malabsorption, which is caused by a number of mechanisms.

Short bowel syndrome is a rare malabsorption disorder caused by a lack of functional small intestine. The primary symptom is diarrhea, which can result in dehydration, malnutrition, and weight loss. Other symptoms may include bloating, heartburn, feeling tired, lactose intolerance, and foul-smelling stool. Complications can include anemia and kidney stones.

Vertical banded gastroplasty (VBG), also known as stomach stapling, is a form of bariatric surgery for weight control. The VBG procedure involves using a band and staples to create a small stomach pouch. In the bottom of the pouch is an approximate one-centimeter hole through which the pouch contents can flow into the remainder of the stomach and hence on to the remainder of the gastrointestinal tract.
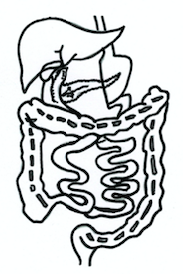
The duodenal switch (DS) procedure, gastric reduction duodenal switch (GRDS), is a weight loss surgery procedure that is composed of a restrictive and a malabsorptive aspect.

A laparoscopic adjustable gastric band, commonly called a lap-band, A band, or LAGB, is an inflatable silicone device placed around the top portion of the stomach to treat obesity, intended to decrease food consumption.

Sleeve gastrectomy or vertical sleeve gastrectomy, is a surgical weight-loss procedure, typically performed laparoscopically, in which approximately 75 - 85% of the stomach is removed, along the greater curvature, which leaves a cylindrical, or "sleeve"-shaped stomach the size of a banana. Weight loss is affected not only through the reduction of the organ's size, but by the removal of the portion of it that produces ghrelin, the hormone that stimulates appetite. Patients can lose 50-70 percent of excess weight over the course of the two years that follow the surgery. The procedure is irreversible, though in some uncommon cases, patients can regain the lost weight, via resumption of deleterious habits, or dilation of the stomach over time, which can require gastric sleeve revision surgery to either repair the sleeve or convert it to another type of weight loss method that may produce better results, such as a gastric bypass or duodenal switch.

Intestinal atresia is any congenital malformation of the structure of the intestine that causes bowel obstruction. The malformation can be a narrowing (stenosis), absence or malrotation of a portion of the intestine. These defects can either occur in the small or large intestine.
Bariatric surgery is the medical term for a variety of procedures dealing with obesity. Long term weight loss through the standard of care procedures is largely achieved by altering gut hormone levels responsible for hunger and satiety, leading to a new hormonal weight set point. Bariatric surgery is the most effective treatment causing weight loss and reducing complications of obesity.
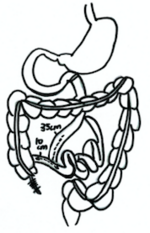
Jejunoileal bypass (JIB) was a surgical weight-loss procedure performed for the relief of morbid obesity from the 1950s through the 1970s in which all but 30 cm (12 in) to 45 cm (18 in) of the small bowel were detached and set to the side.
Revision weight loss surgery is a surgical procedure that is performed on patients who have already undergone a form of bariatric surgery, and have either had complications from such surgery or have not achieved significant weight loss results from the initial surgery. Procedures are usually performed laparoscopically, though open surgery may be required if prior bariatric surgery has resulted in extensive scarring.

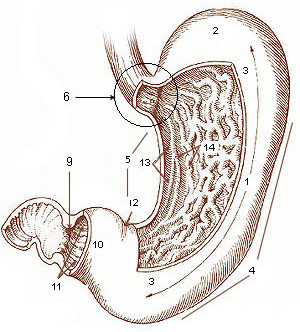
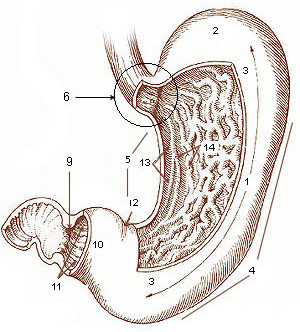
The human digestive system consists of the gastrointestinal tract plus the accessory organs of digestion. Digestion involves the breakdown of food into smaller and smaller components, until they can be absorbed and assimilated into the body. The process of digestion has three stages: the cephalic phase, the gastric phase, and the intestinal phase.

SADI-S is a bariatric surgical technique to address metabolic disorders and to lose weight. It is a variation on the Duodenal Switch surgery, incorporating a vertical sleeve gastrectomy with a gastric bypass technique.
A duodenal-jejunal bypass liner, commonly called an EndoBarrier, is an implantable medical device in the form of a thin flexible 60 cm-long tube that creates a physical barrier between ingested food and the duodenum/proximal jejunum. The duodenal-jejunal bypass liner prevents the interaction of food with enzymes and hormones in the proximal intestine to treat type 2 diabetes and obesity. The duodenal-jejunal bypass liner is delivered endoscopically and has been tested on the morbidly obese as well as obese patients with a BMI less than 40, particularly those with difficult-to-manage type 2 diabetes. Despite a handful of serious adverse events such as gastrointestinal bleeding, abdominal pain, and device migration — all resolved with device removal — initial clinical trials have produced promising results in the treatment's ability to improve weight loss and glucose homeostasis outcomes.
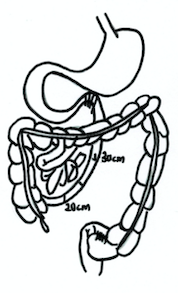
Ileal Interposition is a Metabolic Surgery procedure, used to treat overweight diabetic patients through surgical means. First presented by the Brazilian surgeon Aureo De Paula in 1999, this technique is applied by placing ileum, which is the distal part of the small intestine, either between stomach and the proximal part of the small intestine (1) or by placing the ileum to the proximal part of the small intestine without touching the natural connections of the stomach (2). There are 2 different versions of the operation. Sleeve gastrectomy procedure is standard for both of the versions.
Stomach Intestinal Pylorus-Sparing (SIPS) surgery is a type of weight-loss surgery. It was developed in 2013 by two U.S. surgeons, Daniel Cottam from Utah and Mitchell S. Roslin from New York.
Edward Eaton Mason was an American surgeon, professor, and medical researcher who specialized in obesity surgery. He is known for developing restrictive gastric surgery for morbidly obese patients. Mason introduced the first gastric bypass surgery in 1966 and was the inventor of the first vertical banded gastroplasty surgery in 1980.