Related Research Articles
Insulin resistance (IR) is a pathological condition in which cells either fail to respond normally to the hormone insulin or downregulate insulin receptors in response to hyperinsulinemia.

Abdominal obesity, also known as central obesity and truncal obesity, is the human condition of an excessive concentration of visceral fat around the stomach and abdomen to such an extent that it is likely to harm its bearer's health. Abdominal obesity has been strongly linked to cardiovascular disease, Alzheimer's disease, and other metabolic and vascular diseases.

Lipolysis is the metabolic pathway through which lipid triglycerides are hydrolyzed into a glycerol and free fatty acids. It is used to mobilize stored energy during fasting or exercise, and usually occurs in fat adipocytes. The most important regulatory hormone in lipolysis is insulin; lipolysis can only occur when insulin action falls to low levels, as occurs during fasting. Other hormones that affect lipolysis include glucagon, epinephrine, norepinephrine, growth hormone, atrial natriuretic peptide, brain natriuretic peptide, and cortisol.
Carbohydrate metabolism is the whole of the biochemical processes responsible for the metabolic formation, breakdown, and interconversion of carbohydrates in living organisms.

Adipose tissue (also known as body fat, or simply fat) is a loose connective tissue composed mostly of adipocytes. In addition to adipocytes, adipose tissue contains the stromal vascular fraction(SVF) of cells including preadipocytes, fibroblasts, vascular endothelial cells and a variety of immune cells such as adipose tissue macrophages. Adipose tissue is derived from preadipocytes. Its main role is to store energy in the form of lipids, although it also cushions and insulates the body. Far from being hormonally inert, adipose tissue has, in recent years, been recognized as a major endocrine organ, as it produces hormones such as leptin, estrogen, resistin, and cytokines (especially TNFα). In obesity, adipose tissue is also implicated in the chronic release of pro-inflammatory markers known as adipokines, which are responsible for the development of metabolic syndrome, a constellation of diseases, including type 2 diabetes, cardiovascular disease and atherosclerosis. The two types of adipose tissue are white adipose tissue (WAT), which stores energy, and brown adipose tissue (BAT), which generates body heat. The formation of adipose tissue appears to be controlled in part by the adipose gene. Adipose tissue – more specifically brown adipose tissue – was first identified by the Swiss naturalist Conrad Gessner in 1551.

Adipocytes, also known as lipocytes and fat cells, are the cells that primarily compose adipose tissue, specialized in storing energy as fat. Adipocytes are derived from mesenchymal stem cells which give rise to adipocytes through adipogenesis. In cell culture, adipocyte progenitors can also form osteoblasts, myocytes and other cell types.

Hyperinsulinemia is a condition in which there are excess levels of insulin circulating in the blood relative to the level of glucose. While it is often mistaken for diabetes or hyperglycaemia, hyperinsulinemia can result from a variety of metabolic diseases and conditions, as well as non-nutritive sugars in the diet. While hyperinsulinemia is often seen in people with early stage type 2 diabetes mellitus, it is not the cause of the condition and is only one symptom of the disease. Type 1 diabetes only occurs when pancreatic beta-cell function is impaired. Hyperinsulinemia can be seen in a variety of conditions including diabetes mellitus type 2, in neonates and in drug-induced hyperinsulinemia. It can also occur in congenital hyperinsulinism, including nesidioblastosis.
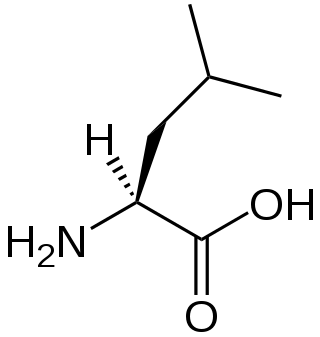
A branched-chain amino acid (BCAA) is an amino acid having an aliphatic side-chain with a branch. Among the proteinogenic amino acids, there are three BCAAs: leucine, isoleucine, and valine. Non-proteinogenic BCAAs include 2-aminoisobutyric acid and alloisoleucine.
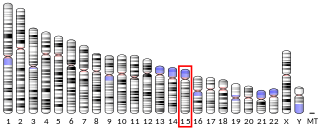
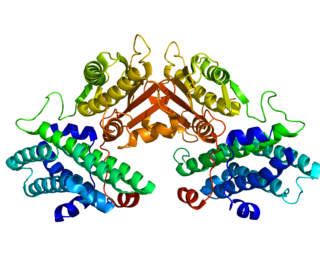
Glucose transporter type 4 (GLUT4), also known as solute carrier family 2, facilitated glucose transporter member 4, is a protein encoded, in humans, by the SLC2A4 gene. GLUT4 is the insulin-regulated glucose transporter found primarily in adipose tissues and striated muscle. The first evidence for this distinct glucose transport protein was provided by David James in 1988. The gene that encodes GLUT4 was cloned and mapped in 1989.
Perilipin, also known as lipid droplet-associated protein, perilipin 1, or PLIN, is a protein that, in humans, is encoded by the PLIN gene. The perilipins are a family of proteins that associate with the surface of lipid droplets. Phosphorylation of perilipin is essential for the mobilization of fats in adipose tissue.
Intramuscular fat is located inside skeletal muscle fibers. It is stored in lipid droplets that exist in close proximity to the mitochondria, where it serves as an energy store that can be used during exercise. In humans, excess accumulation of intramuscular fat has been associated with conditions such as insulin resistance and type 2 diabetes. The human immunodeficiency virus (HIV)-lipodystrophy syndrome is associated with over-accumulation of intramuscular fat, which may contribute to AIDS wasting syndrome.
Starvation response in animals is a set of adaptive biochemical and physiological changes, triggered by lack of food or extreme weight loss, in which the body seeks to conserve energy by reducing the amount of food energy it consumes.
The Randle cycle, also known as the glucose fatty-acid cycle, is a metabolic process involving the competition of glucose and fatty acids for substrates. It is theorized to play a role in explaining type 2 diabetes and insulin resistance.

The fatty-acid-binding proteins (FABPs) are a family of transport proteins for fatty acids and other lipophilic substances such as eicosanoids and retinoids. These proteins are thought to facilitate the transfer of fatty acids between extra- and intracellular membranes. Some family members are also believed to transport lipophilic molecules from outer cell membrane to certain intracellular receptors such as PPAR. The FABPs are intracellular carriers that “solubilize” the endocannabinoid anandamide (AEA), transporting AEA to the breakdown by FAAH, and compounds that bind to FABPs block AEA breakdown, raising its level. The cannabinoids are also discovered to bind human FABPs that function as intracellular carriers, as THC and CBD inhibit the cellular uptake and catabolism of AEA by targeting FABPs. Competition for FABPs may in part or wholly explain the increased circulating levels of endocannabinoids reported after consumption of cannabinoids. Levels of fatty-acid-binding protein have been shown to decline with ageing in the mouse brain, possibly contributing to age-associated decline in synaptic activity.
Pyruvate dehydrogenase lipoamide kinase isozyme 4, mitochondrial (PDK4) is an enzyme that in humans is encoded by the PDK4 gene. It codes for an isozyme of pyruvate dehydrogenase kinase.
Lipid droplets, also referred to as lipid bodies, oil bodies or adiposomes, are lipid-rich cellular organelles that regulate the storage and hydrolysis of neutral lipids and are found largely in the adipose tissue. They also serve as a reservoir for cholesterol and acyl-glycerols for membrane formation and maintenance. Lipid droplets are found in all eukaryotic organisms and store a large portion of lipids in mammalian adipocytes. Initially, these lipid droplets were considered to merely serve as fat depots, but since the discovery in the 1990s of proteins in the lipid droplet coat that regulate lipid droplet dynamics and lipid metabolism, lipid droplets are seen as highly dynamic organelles that play a very important role in the regulation of intracellular lipid storage and lipid metabolism. The role of lipid droplets outside of lipid and cholesterol storage has recently begun to be elucidated and includes a close association to inflammatory responses through the synthesis and metabolism of eicosanoids and to metabolic disorders such as obesity, cancer, and atherosclerosis. In non-adipocytes, lipid droplets are known to play a role in protection from lipotoxicity by storage of fatty acids in the form of neutral triacylglycerol, which consists of three fatty acids bound to glycerol. Alternatively, fatty acids can be converted to lipid intermediates like diacylglycerol (DAG), ceramides and fatty acyl-CoAs. These lipid intermediates can impair insulin signaling, which is referred to as lipid-induced insulin resistance and lipotoxicity. Lipid droplets also serve as platforms for protein binding and degradation. Finally, lipid droplets are known to be exploited by pathogens such as the hepatitis C virus, the dengue virus and Chlamydia trachomatis among others.
Lipotoxicity is a metabolic syndrome that results from the accumulation of lipid intermediates in non-adipose tissue, leading to cellular dysfunction and death. The tissues normally affected include the kidneys, liver, heart and skeletal muscle. Lipotoxicity is believed to have a role in heart failure, obesity, and diabetes, and is estimated to affect approximately 25% of the adult American population.
The Summermatter cycle is a physiological concept describing the complex relationship between physical activity/inactivity and energy expenditure/conservation.
Hepatokines are proteins produced by liver cells (hepatocytes) that are secreted into the circulation and function as hormones across the organism. Research is mostly focused on hepatokines that play a role in the regulation of metabolic diseases such as diabetes and fatty liver and include: Adropin, ANGPTL4, Fetuin-A, Fetuin-B, FGF-21, Hepassocin, LECT2, RBP4,Selenoprotein P, Sex hormone-binding globulin.
Deborah Marie Muoio is the George Barth Geller Distinguished Professor of Cardiovascular Disease at Duke University. She is known for her work on diabetes, obesity, and metabolism.
References
- ↑ Schrauwen-Hinderling VB, van Loon LJ, Koopman R, Nicolay K, Saris WH, Kooi ME (December 1, 2003). "Intramyocellular lipid content is increased after exercise in nonexercising human skeletal muscle". Journal of Applied Physiology. 95 (6): 2328–2332. doi:10.1152/japplphysiol.00304.2003. PMID 12923116.
- ↑ Guo ZK (2007). "Intramyocellular lipid kinetics and insulin resistance". Lipids Health Dis. 6: 18. doi: 10.1186/1476-511X-6-18 . PMC 1971250 . PMID 17650308.
- ↑ Greco AV, Mingrone G, Giancaterini A, Manco M, Morroni M, Cinti S, Granzotto M, Vettor R, Camastra S, Ferrannini E (2002). "Insulin resistance in morbid obesity: reversal with intramyocellular fat depletion". Diabetes. 51 (1): 144–51. doi: 10.2337/diabetes.51.1.144 . PMID 11756334.