
Jawahar L. Mehta is the Stebbins Chair and Professor of Medicine at the College of Medicine, University of Arkansas for Medical Sciences (UAMS).

Jawahar L. Mehta is the Stebbins Chair and Professor of Medicine at the College of Medicine, University of Arkansas for Medical Sciences (UAMS).
Mehta was born in India and migrated to the United States in 1970. He received his M.D. from Punjab University in 1968 and PhD from the University of Uppsala, Uppsala, Sweden. [1] Mehta's thesis topic was "studies on experimental myocardial reperfusion" [2] which he completed under the direction of Prof. Tom Saldeen. He completed his post-graduate training in Medicine at the Mount Sinai Medical Center in New York, followed by a research fellowship at the University of Minnesota, Minneapolis. His first faculty position was at the University of Florida, where he rose to be Professor of Medicine. He was appointed the Stebbins Chair and Professor of Medicine and Director of Cardiovascular Medicine at the College of Medicine, University of Arkansas for Medical Sciences (UAMS) in October 2000. [3] He is currently also an Adjunct Faculty Member at the University of Arkansas, Clinton School of Public Service.
At the University of Florida College of Medicine, Mehta was among the first [4] to describe platelet activation as a basis of acute coronary syndromes. Later, he went on to show that platelets also have a protective effect on the heart during ischemia mediated through release of transforming growth factor ß1. Together with Prof. Ian Phillips, he directed the hypertension center at the University of Florida. His current research is on the uptake of oxidized low density lipoprotein (LDL) by specialized receptors LOX-1 (OLR1).
Mehta has made clinical and basic research contributions to the pathobiology of cardiovascular diseases (h index 101, 81,016 citations). [5] His work on LOX-1 receptors, its polymorphic variants and its role in atherogenesis and myocardial ischemia has led to new therapeutic targets now being pursued by several biotech companies, such as MedImmune.
He is a member of the American Society for Clinical Investigation, American Association of Physicians, and the Association of University Cardiologists. [6] His research has been described as "unparalleled." [7]
He is also the director of the Molecular Cardiology Program at the University of Arkansas for Medical Sciences [8] and adjunct professor at the University of Rome, Tor Vergata.
Mehta delivered the Swan Memorial Lecture at the World Congress of Cardiology, Vancouver in July 2012. [7] He has been recognized as a Distinguished Fellow by the International Academy of Cardiology, July 2014. He also received the International Pericle d’Oro Prize, University Magna Graecia of Catanzaro, Italy May 2014. [9] In December 2017, Mehta was recognized by Forbes Magazine as one of the top 27 cardiologists in the United States. [10] In April 2018, the University of Arkansas for Medical Sciences honored Mehta by naming him Distinguished Professor, [11] a recognition given to "honor exemplary faculty members who have helped to shape the institution." [12] Grateful patients have established "Mehta/Stebbins Chair in Cardiovascular Research" in his honor. [13] In addition, there is a Jay and Paulette Mehta Visiting Lectureship established in his and his wife's honor at the University of Arkansas for Medical Sciences, Little Rock, Arkansas. [14] The International Academy of Cardiovascular Sciences awarded Dr. Mehta the Lifetime Achievement in Cardiovascular Science, Medicine, and Surgery in 2019 at its annual meeting in Vrnjacka Banja, Serbia. [15] In the same year, the Italian Society of Cardiology and the University of Rome Tor Vergata honored him with Distinguished Professorship and Lifetime Achievement Award. [16]
In 2020, the Department of Veterans Affairs honored Dr. Mehta with the Senior Clinician Scientist Investigator (SCSI) Award in Cardiovascular Sciences. [17] Later that same year, the University of Arkansas for Medical Sciences unveiled the Drs. Paulette and Jay Mehta Award in Creative Writing. [18]
Dr. Mehta is married to Paulette Mehta, MD, an oncologist in Little Rock, Arkansas. His children include Asha Mehta of Boston, Massachusetts and Jason Mehta of Tampa, Florida. His grandchildren include Jasper Garg, Griffen Garg, Maia Mehta, Jack Mehta, and Zara Garg.

Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of atherosclerotic plaque in the arteries of the heart. It is the most common of the cardiovascular diseases. Types include stable angina, unstable angina, and myocardial infarction. A common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw. Occasionally it may feel like heartburn. Usually symptoms occur with exercise or emotional stress, last less than a few minutes, and improve with rest. Shortness of breath may also occur and sometimes no symptoms are present. In many cases, the first sign is a heart attack. Other complications include heart failure or an abnormal heartbeat.

Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.
An antiplatelet drug (antiaggregant), also known as a platelet agglutination inhibitor or platelet aggregation inhibitor, is a member of a class of pharmaceuticals that decrease platelet aggregation and inhibit thrombus formation. They are effective in the arterial circulation where classical Vitamin K antagonist anticoagulants have minimal effect.

Reperfusion injury, sometimes called ischemia-reperfusion injury (IRI) or reoxygenation injury, is the tissue damage caused when blood supply returns to tissue after a period of ischemia or lack of oxygen. The absence of oxygen and nutrients from blood during the ischemic period creates a condition in which the restoration of circulation results in inflammation and oxidative damage through the induction of oxidative stress rather than restoration of normal function.

Coronary thrombosis is defined as the formation of a blood clot inside a blood vessel of the heart. This blood clot may then restrict blood flow within the heart, leading to heart tissue damage, or a myocardial infarction, also known as a heart attack.
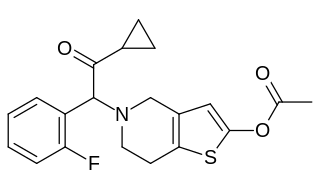
Prasugrel, sold under the brand name Effient in the US, Australia and India, and Efient in the EU) is a medication used to prevent formation of blood clots. It is a platelet inhibitor and an irreversible antagonist of P2Y12 ADP receptors and is of the thienopyridine drug class. It was developed by Daiichi Sankyo Co. and produced by Ube and marketed in the United States in cooperation with Eli Lilly and Company.

P2Y12 is a chemoreceptor for adenosine diphosphate (ADP) that belongs to the Gi class of a group of G protein-coupled (GPCR) purinergic receptors. This P2Y receptor family has several receptor subtypes with different pharmacological selectivity, which overlaps in some cases, for various adenosine and uridine nucleotides. The P2Y12 receptor is involved in platelet aggregation and is thus a biological target for the treatment of thromboembolisms and other clotting disorders. Two transcript variants encoding the same isoform have been identified for this gene.
Coronary vasospasm refers to when a coronary artery suddenly undergoes either complete or sub-total temporary occlusion.
Myocardial stunning or transient post-ischemic myocardial dysfunction is a state of mechanical cardiac dysfunction that can occur in a portion of myocardium without necrosis after a brief interruption in perfusion, despite the timely restoration of normal coronary blood flow. In this situation, even after ischemia has been relieved and myocardial blood flow (MBF) returns to normal, myocardial function is still depressed for a variable period of time, usually days to weeks. This reversible reduction of function of heart contraction after reperfusion is not accounted for by tissue damage or reduced blood flow, but rather, its thought to represent a perfusion-contraction "mismatch". Myocardial stunning was first described in laboratory canine experiments in the 1970s where LV wall abnormalities were observed following coronary artery occlusion and subsequent reperfusion.

Accelerated idioventricular rhythm is a ventricular rhythm with a rate of between 40 and 120 beats per minute. Idioventricular means “relating to or affecting the cardiac ventricle alone” and refers to any ectopic ventricular arrhythmia. Accelerated idioventricular arrhythmias are distinguished from ventricular rhythms with rates less than 40 and those faster than 120. Though some other references limit to between 60 and 100 beats per minute. It is also referred to as AIVR and "slow ventricular tachycardia."

Myocardial perfusion imaging or scanning is a nuclear medicine procedure that illustrates the function of the heart muscle (myocardium).

Oxidized low-density lipoprotein receptor 1 also known as lectin-type oxidized LDL receptor 1 (LOX-1) is a protein that in humans is encoded by the OLR1 gene.

Valentín Fuster Carulla, 1st Marquess of Fuster is a Spanish cardiologist and aristocrat.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat, feeling tired, and decreased level of consciousness. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.

Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack. Reperfusion therapy includes drugs and surgery. The drugs are thrombolytics and fibrinolytics used in a process called thrombolysis. Surgeries performed may be minimally-invasive endovascular procedures such as a percutaneous coronary intervention (PCI), which involves coronary angioplasty. The angioplasty uses the insertion of a balloon and/or stents to open up the artery. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.

Management of acute coronary syndrome is targeted against the effects of reduced blood flow to the affected area of the heart muscle, usually because of a blood clot in one of the coronary arteries, the vessels that supply oxygenated blood to the myocardium. This is achieved with urgent hospitalization and medical therapy, including drugs that relieve chest pain and reduce the size of the infarct, and drugs that inhibit clot formation; for a subset of patients invasive measures are also employed. Basic principles of management are the same for all types of acute coronary syndrome. However, some important aspects of treatment depend on the presence or absence of elevation of the ST segment on the electrocardiogram, which classifies cases upon presentation to either ST segment elevation myocardial infarction (STEMI) or non-ST elevation acute coronary syndrome (NST-ACS); the latter includes unstable angina and non-ST elevation myocardial infarction (NSTEMI). Treatment is generally more aggressive for STEMI patients, and reperfusion therapy is more often reserved for them. Long-term therapy is necessary for prevention of recurrent events and complications.

Cariporide is a selective Na+/H+ exchange inhibitor. Cariporide has been shown to actively suppress the cell death caused by oxidative stress.
Cardioprotection includes all mechanisms and means that contribute to the preservation of the heart by reducing or even preventing myocardial damage. Cardioprotection encompasses several regimens that have shown to preserve function and viability of cardiac muscle cell tissue subjected to ischemic insult or reoxygenation. Cardioprotection includes strategies that are implemented before an ischemic event, during an ischemic event and after the event and during reperfusion. These strategies can be further stratified by performing the intervention locally or remotely, creating classes of conditioning known as remote ischemic PC (RIPC), remote ischemic PostC and remote ischemic PerC. Classical (local) preconditioning has an early phase with an immediate onset lasting 2–3 hours that protects against myocardial infarction. The early phase involves post-translational modification of preexisting proteins, brought about by the activation of G protein-coupled receptors as well as downstream MAPK's and PI3/Akt. These signaling events act on the ROS-generating mitochondria, activate PKCε and the Reperfusion Injury Salvage Kinase (RISK) pathway, preventing mitochondrial permeability transition pore (MTP) opening. The late phase with an onset of 12–24 hours that lasts 3–4 days and protects against both infarction and reversible postischemic contractile dysfunction, termed myocardial stunning. This phase involves the synthesis of new cardioprotective proteins stimulated by nitric oxide (NO), ROS and adenosine acting on kinases such as PKCε and Src, which in turn activate gene transcription and upregulation of late PC molecular players.
Gerd Heusch is a German physician, physiologist, and professor as well as chair of the Institute for Pathophysiology at the University of Essen Medical School.