Related Research Articles

Syringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. Often, syringomyelia is used as a generic term before an etiology is determined. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in loss of feeling, paralysis, weakness, and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. It may also lead to a cape-like bilateral loss of pain and temperature sensation along the upper chest and arms. The combination of symptoms varies from one patient to another depending on the location of the syrinx within the spinal cord, as well as its extent.

Back pain is pain felt in the back. It may be classified as neck pain (cervical), middle back pain (thoracic), lower back pain (lumbar) or coccydynia based on the segment affected. The lumbar area is the most common area affected. An episode of back pain may be acute, subacute or chronic depending on the duration. The pain may be characterized as a dull ache, shooting or piercing pain or a burning sensation. Discomfort can radiate to the arms and hands as well as the legs or feet, and may include numbness or weakness in the legs and arms.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

Vertebral augmentation, including vertebroplasty and kyphoplasty, refers to similar percutaneous spinal procedures in which bone cement is injected through a small hole in the skin into a fractured vertebra in order to relieve back pain caused by a vertebral compression fracture. After decades of medical research into the efficacy and safety of vertebral augmentation, there is still a lack of consensus regarding certain aspects of vertebroplasty and kyphoplasty.

Low back pain (LBP) or lumbago is a common disorder involving the muscles, nerves, and bones of the back, in between the lower edge of the ribs and the lower fold of the buttocks. Pain can vary from a dull constant ache to a sudden sharp feeling. Low back pain may be classified by duration as acute, sub-chronic, or chronic. The condition may be further classified by the underlying cause as either mechanical, non-mechanical, or referred pain. The symptoms of low back pain usually improve within a few weeks from the time they start, with 40–90% of people recovered by six weeks.

Back injuries result from damage, wear, or trauma to the bones, muscles, or other tissues of the back. Common back injuries include sprains and strains, herniated discs, and fractured vertebrae. The lumbar spine is often the site of back pain. The area is susceptible because of its flexibility and the amount of body weight it regularly bears. It is estimated that low-back pain may affect as much as 80 to 90 percent of the general population in the United States.

Spinal fusion, also called spondylodesis or spondylosyndesis, is a neurosurgical or orthopedic surgical technique that joins two or more vertebrae. This procedure can be performed at any level in the spine and prevents any movement between the fused vertebrae. There are many types of spinal fusion and each technique involves using bone grafting—either from the patient (autograft), donor (allograft), or artificial bone substitutes—to help the bones heal together. Additional hardware is often used to hold the bones in place while the graft fuses the two vertebrae together. The placement of hardware can be guided by fluoroscopy, navigation systems, or robotics.
Middle back pain, also known as thoracic back pain, is back pain that is felt in the region of the thoracic vertebrae, which are between the bottom of the neck and top of the lumbar spine. It has a number of potential causes, ranging from muscle strain to collapse of a vertebra or rare serious diseases. The upper spine is very strong and stable to support the weight of the upper body, as well as to anchor the rib cage which provides a cavity to allow the heart and lungs to function and protect them.

A spinal cord stimulator (SCS) or dorsal column stimulator (DCS) is a type of implantable neuromodulation device that is used to send electrical signals to select areas of the spinal cord for the treatment of certain pain conditions. SCS is a consideration for people who have a pain condition that has not responded to more conservative therapy. There are also spinal cord stimulators under research and development that could enable patients with spinal cord injury to walk again via epidural electrical stimulation (EES).
Failed back syndrome or post-laminectomy syndrome is a condition characterized by chronic pain following back surgeries. Many factors can contribute to the onset or development of FBS, including residual or recurrent spinal disc herniation, persistent post-operative pressure on a spinal nerve, altered joint mobility, joint hypermobility with instability, scar tissue (fibrosis), depression, anxiety, sleeplessness, spinal muscular deconditioning and even Cutibacterium acnes infection. An individual may be predisposed to the development of FBS due to systemic disorders such as diabetes, autoimmune disease and peripheral blood vessels (vascular) disease.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.
Manipulation under anesthesia (MUA) or fibrosis release procedures is a multidisciplinary, chronic pain-related manual therapy modality which is used for the purpose of improving articular and soft tissue movement. This is accomplished by way of a combination of controlled joint mobilization/manipulation and myofascial release techniques. MUA is used by osteopathic/orthopedic physicians, chiropractors and specially trained physicians. It aims to break up adhesions on or around spinal joints or extremity joints to which a restricted range of motion can be painful and limit function. Failed attempts at other standard conservative treatment methods, over a sufficient time-frame, is one of the principal patient qualifiers.

A compression fracture is a collapse of a vertebra. It may be due to trauma or due to a weakening of the vertebra. This weakening is seen in patients with osteoporosis or osteogenesis imperfecta, lytic lesions from metastatic or primary tumors, or infection. In healthy patients, it is most often seen in individuals suffering extreme vertical shocks, such as ejecting from an ejection seat. Seen in lateral views in plain x-ray films, compression fractures of the spine characteristically appear as wedge deformities, with greater loss of height anteriorly than posteriorly and intact pedicles in the anteroposterior view.
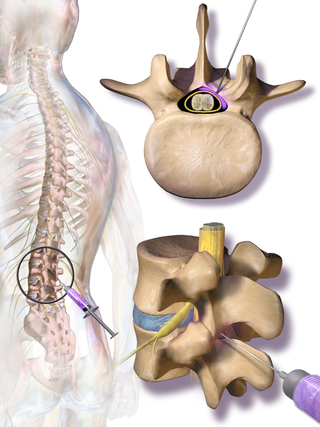
Epidural steroid injection (ESI) is a technique in which corticosteroids and a local anesthetic are injected into the epidural space around the spinal cord in an effort to improve spinal stenosis, spinal disc herniation, or both. It is of benefit with a rare rate of major side effects.
Interventional pain management or interventional pain medicine is a medical subspecialty defined by the National Uniforms Claims Committee (NUCC) as, " invasive interventions such as the discipline of medicine devoted to the diagnosis and treatment of pain related disorders principally with the application of interventional techniques in managing sub acute, chronic, persistent, and intractable pain, independently or in conjunction with other modalities of treatment". Medicare Payment Advisory Commission (MedPAC) defined interventional techniques as, "minimally invasive procedures including, percutaneous precision needle placement, with placement of drugs in targeted areas or ablation of targeted nerves; and some surgical techniques such as laser or endoscopic diskectomy, intrathecal infusion pumps and spinal cord stimulators, for the diagnosis and management of chronic, persistent or intractable pain". Minimally invasive interventions such as facet joint injections, nerve blocks, neuroaugmentation, vertebroplasty, kyphoplasty, nucleoplasty, endoscopic discectomy, and implantable drug delivery systems are utilized in managing subacute or chronic pain.
Minimally invasive spine surgery, also known as MISS, has no specific meaning or definition. It implies a lack of severe surgical invasion. The older style of open-spine surgery for a relatively small disc problem used to require a 5-6 inch incision and a month in the hospital. MISS techniques utilize more modern technology, advanced imaging techniques and special medical equipment to reduce tissue trauma, bleeding, radiation exposure, infection risk, and decreased hospital stays by minimizing the size of the incision. Modern endoscopic procedures can be done through a 2 to 5 mm skin opening. By contrast, procedures done with a microscope require skin openings of approximately one inch, or more.
Laxmaiah Manchikanti is an Indian American physician and anesthesiologist specializing in interventional pain management, professor, philanthropist, and author. He is the founder of the American Society of Interventional Pain Physicians (ASIPP), the Society of Interventional Pain Management Surgery Centers (SIPMS) and the Pain Physician, a newspaper owned by his organization, Manchikanti has served as clinical professor of Anesthesiology and Perioperative Medicine at the University of Louisville School of Medicine. He has served as chairman of the board and chief executive officer of ASIPP since 1998. He has been medical director of the Pain Management Centers of Paducah, Kentucky and Marion, Illinois and the Ambulatory Surgery Center in Paducah, Kentucky since 1992. He co-founded a multistate national company, Pain Management Centers of America (PMCOA), in 2019 with Mahendra Sanapati, MD.

Gábor Béla Rácz, is a Hungarian-American board-certified anesthesiologist and professor emeritus at Texas Tech University Health Science Center (TTUHSC) in Lubbock, Texas, where he is also Chairman Emeritus of the Department of Anesthesiology and Co-Director of Pain Services. He has worked in the field of chronic back pain and complex regional pain syndrome (CRPS).
DFINE, Inc. was an American medical device company with headquarters in San Jose, California. It was known for its development of minimally invasive therapeutic devices built upon a radiofrequency platform for the treatment of spinal diseases. The platform included two applications, the StabiliT Vertebral Augmentation System for the treatment of vertebral compression fractures and the STAR Tumor Ablation System for pain relief treatment of metastatic spinal tumors.
Epidural lysis of adhesions (LOA), also known as percutaneous adhesiolysis or the Racz procedure, is a minimally invasive spine surgery which involves the dissolution of epidural scar tissue by mechanical means to facilitate the spread of analgesics in an effort to alleviate pain. It is a type of percutaneous adhesiolysis procedure commonly used to treat chronic pain resulting from failed back surgery syndrome wherein scar tissue has formed around the nerves and causes pain. Evidence suggests the procedure may also be effective in treating spinal stenosis and radicular pain caused by a herniated disc.
References
- ↑ "Five Physicians Join Rush; New Vertebroplasty Study; Need Surgery? Name Your Price! | Orthopedics This Week". ryortho.com. Retrieved 2022-10-31.
- 1 2 Kolata, Gina (24 January 2019). "Spinal Fractures Can Be Terribly Painful. A Common Treatment Isn't Helping". The New York Times.
- ↑ Manchikanti, Laxmaiah; Kaye, Alan D.; Falco, Frank J.E.; Hirsch, Joshua A., eds. (2018). Essentials of Interventional Techniques in Managing Chronic Pain. doi:10.1007/978-3-319-60361-2. ISBN 978-3-319-60359-9. S2CID 33207028.[ page needed ][ non-primary source needed ]
- ↑ González, R. Gilberto; Hirsch, Joshua A.; Lev, Michael H.; Schaefer, Pamela W.; Schwamm, Lee H., eds. (2011). Acute Ischemic Stroke. doi:10.1007/978-3-642-12751-9. ISBN 978-3-642-12750-2.[ page needed ][ non-primary source needed ]
- ↑ Manchikanti, Laxmaiah; Kaye, Alan D.; Falco, Frank J.E.; Hirsch, Joshua A., eds. (2018). Essentials of Interventional Techniques in Managing Chronic Pain. doi:10.1007/978-3-319-60361-2. ISBN 978-3-319-60359-9. S2CID 33207028.[ non-primary source needed ][ page needed ]
- ↑ Hirsch, Joshua A; Barr, John D; Zoarski, Gregg H (September 2013). "Sacroplasty: beyond the beginning". Journal of NeuroInterventional Surgery. 5 (5): 395. doi:10.1136/neurintsurg-2012-010434. PMID 22753269. S2CID 38378700.[ non-primary source needed ]
- 1 2 "Joshua A. Hirsch, MD". SpineUniverse.
- ↑ Chandra, R.V.; Maingard, J.; Asadi, H.; Slater, L.-A.; Mazwi, T.-L.; Marcia, S.; Barr, J.; Hirsch, J.A. (May 2018). "Vertebroplasty and Kyphoplasty for Osteoporotic Vertebral Fractures: What Are the Latest Data?". American Journal of Neuroradiology. 39 (5): 798–806. doi:10.3174/ajnr.A5458. PMC 7410658 . PMID 29170272.[ non-primary source needed ]
- ↑ Prestigiacomo, Charles J.; Duffis, E. Jesús; Gandhi, Chirag D., eds. (2015). "Principles of Vertebroplasty". Surgical Endovascular Neuroradiology. doi:10.1055/b-0034-99125. ISBN 978-1-60406-057-7.[ non-primary source needed ]
- ↑ Carlson, Matt (2011). "Journalists Fight Back: Newsweek and the Koran Abuse Story". On the Condition of Anonymity. Vol. 1. doi:10.5406/illinois/9780252035999.003.0004. ISBN 978-0-252-03599-9.
- ↑ Spetzler, Robert F.; Kondziolka, Douglas S.; Higashida, Randall T.; Kalani, M. Yashar S., eds. (2014). Comprehensive Management of Arteriovenous Malformations of the Brain and Spine. doi:10.1017/CBO9781139523943. ISBN 978-1-139-52394-3.[ page needed ][ non-primary source needed ]
- ↑ Kolata, Gina (28 August 2005). "Spinal Cement Draws Patients and Questions". The New York Times.
- ↑ Gonzalez, L. Fernando; Albuquerque, Felipe C.; McDougall, Cameron G., eds. (2015). Neurointerventional Techniques. doi:10.1055/b-002-102503. ISBN 978-1-60406-757-6.
- ↑ "Joshua Hirsch, MD -". Massachusetts General Hospital. Retrieved 2022-10-28.
- 1 2 Hirsh, Joshua (2017-07-18). "Joshua A Hirsch". NeuroNews International (Interview). Retrieved 2022-10-28.
- ↑ "Dr. Joshua A. Hirsch, MD | Boston, MA | Radiologist | US News Doctors".
- ↑ González, R. Gilberto; Hirsch, Joshua A.; Lev, Michael H.; Schaefer, Pamela W.; Schwamm, Lee H., eds. (2011). Acute Ischemic Stroke. doi:10.1007/978-3-642-12751-9. ISBN 978-3-642-12750-2.[ page needed ]
- 1 2 "Joshua A Hirsch, M.D. | Mass General Research Institute". Find a Researcher - Massachusetts General Hospital. Retrieved 2022-10-28.
- ↑ "Editorial Board". Journal of NeuroInterventional Surgery. Retrieved 2022-10-28.
- ↑ "Joshua Hirsch | Harvard Catalyst Profiles". Harvard Catalyst . Retrieved 2022-10-28.
- ↑ "Epidural Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Comprehensive Evidence-Based Guidelines". Pain Physician Journal (Epidural Guidelines).
- ↑ Manchikanti, Laxmaiah (14 May 2020). "Comprehensive Evidence-Based Guidelines for Facet Joint Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines". Pain Physician. 3S, 23 (5, 3S): S1–S127. doi: 10.36076/ppj.2020/23/s1 . S2CID 219398427.
- ↑ Manchikanti, Laxmaiah; Abdi, Salahadin; Atluri, Sairam; Balog, Carl C.; Benyamin, Ramsin M.; Boswell, Mark V.; Brown, Keith R.; Bruel, Brian Mendoza; Bryce, David A.; Burks, Patricia A.; Burton, Allen W.; Calodney, Aaron K.; Caraway, David L.; Cash, Kimberly A.; Christo, Paul J.; Damron, Kim S.; Datta, Sukdeb; Deer, Timothy R.; Diwan, Sudhir; Eriator, Ike; Falco, Frank J.E.; Fellows, Bert; Geffert, Stephanie; Gharibo, Christopher G.; Glaser, Scott E.; Grider, Jay S.; Hameed, Haroon; Hameed, Mariam; Hansen, Hans; Harned, Michael E.; Hayek, Salim M.; Helm, Standiford; Hirsch, Joshua A.; Janata, Jeffrey W.; Kaye, Alan D.; Kaye, Adam M.; Kloth, David S.; Koyyalagunta, Dhanalakshmi; Lee, Marion; Malla, Yogesh; Manchikanti, Kavita N.; McManus, Carla D.; Pampati, Vidyasagar; Parr, Allan T.; Pasupuleti, Ramarao; Patel, Vikram B.; Sehgal, Nalini; Silverman, Sanford M.; Singh, Vijay; Smith, Howard S.; Snook, Lee T.; Solanki, Daneshvari R.; Tracy, Deborah H.; Vallejo, Ricardo; Wargo, Bradley W. (July 2012). "American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2 – guidance". Pain Physician. 15 (3 Suppl): S67–116. PMID 22786449. ProQuest 2655995162.