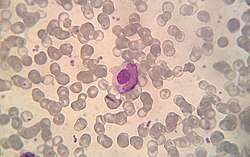
A lupus erythematosus cell (LE cell), also known as Hargraves cell, is a neutrophil or macrophage that has phagocytized (engulfed) the denatured nuclear material of another cell. [1] The denatured material is an absorbed hematoxylin body (also called an LE body). [2]
They are a characteristic of lupus erythematosus, [3] but also found in similar connective tissue disorders or some autoimmune diseases like in severe rheumatoid arthritis. LE cells can be observed in drug-induced lupus, for example, following treatment with methyldopa. [4]
The LE cell was discovered in bone marrow in 1948 by Malcolm McCallum Hargraves (1903–1982), a physician and practicing histologist at the Mayo Clinic . [5] Hargraves may have gained priority by suppressing a publication draft of John R. Haserick, who credits Dorothy Sundberg, chief hematologist at the University of Minnesota Hospitals, with first identifying LE cells. [6]
Classically, the LE cell is analyzed microscopically, but it is also possible to investigate this phenomenon by flow cytometry. [7]
LE cells shouldn't be confused with Tart cells which have engulfed nuclear material, but with a visible chromatin rather than homogeneous appearance. [8]