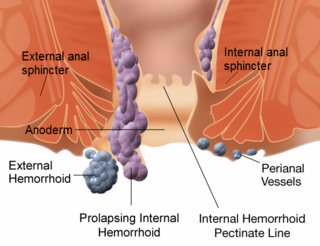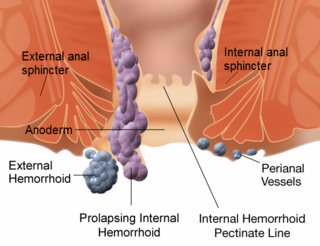
Hemorrhoids, also known as piles, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool control. They become a disease when swollen or inflamed; the unqualified term "hemorrhoid" is often used to refer to the disease. The signs and symptoms of hemorrhoids depend on the type present. Internal hemorrhoids often result in painless, bright red rectal bleeding when defecating. External hemorrhoids often result in pain and swelling in the area of the anus. If bleeding occurs it is usually darker. Symptoms frequently get better after a few days. A skin tag may remain after the healing of an external hemorrhoid.

Fecal incontinence (FI), or in some forms encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits, and receptive anal sex. An estimated 2.2% of community dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.

Rhinoplasty, commonly known as a nose job, is a plastic surgery procedure for altering and reconstructing the nose. There are two types of plastic surgery used – reconstructive surgery that restores the form and functions of the nose and cosmetic surgery that changes the appearance of the nose. Reconstructive surgery seeks to resolve nasal injuries caused by various traumas including blunt, and penetrating trauma and trauma caused by blast injury. Reconstructive surgery also treats birth defects, breathing problems, and failed primary rhinoplasties. Rhinoplasty may remove a bump, narrow nostril width, change the angle between the nose and the mouth, or address injuries, birth defects, or other problems that affect breathing, such as a deviated nasal septum or a sinus condition.

Episiotomy, also known as perineotomy, is a surgical incision of the perineum and the posterior vaginal wall generally done by a midwife or obstetrician. Episiotomy is usually performed during second stage of labor to quickly enlarge the opening for the baby to pass through. The incision, which can be done from the posterior midline of the vulva straight toward the anus or at an angle to the right or left, is performed under local anesthetic, and is sutured after delivery.
An anal fissure is a break or tear in the skin of the anal canal. Anal fissures may be noticed by bright red anal bleeding on toilet paper and undergarments, or sometimes in the toilet. If acute they are painful after defecation, but with chronic fissures, pain intensity often reduces. Anal fissures usually extend from the anal opening and are usually located posteriorly in the midline, probably because of the relatively unsupported nature and poor perfusion of the anal wall in that location. Fissure depth may be superficial or sometimes down to the underlying sphincter muscle. Untreated fissures develop a hood-like skin tag which cover the fissure and cause discomfort and pain.
Otoplasty denotes the surgical and non-surgical procedures for correcting the deformities and defects of the pinna, and for reconstructing a defective, or deformed, or absent external ear, consequent to congenital conditions and trauma. The otoplastic surgeon corrects the defect or deformity by creating an external ear that is of natural proportions, contour, and appearance, usually achieved by the reshaping, the moving, and the augmenting of the cartilaginous support framework of the pinna. Moreover, the occurrence of congenital ear deformities occasionally overlaps with other medical conditions.

Ileostomy is a stoma constructed by bringing the end or loop of small intestine out onto the surface of the skin, or the surgical procedure which creates this opening. Intestinal waste passes out of the ileostomy and is collected in an external ostomy system which is placed next to the opening. Ileostomies are usually sited above the groin on the right hand side of the abdomen.

A facelift, technically known as a rhytidectomy, is a type of cosmetic surgery procedure used to give a more youthful facial appearance. There are multiple surgical techniques and exercise routines. Surgery usually involves the removal of excess facial skin, with or without the tightening of underlying tissues, and the redraping of the skin on the patient's face and neck. Exercise routines tone underlying facial muscles without surgery. Surgical facelifts are effectively combined with eyelid surgery (blepharoplasty) and other facial procedures and are typically performed under general anesthesia or deep twilight sleep.

Blepharoplasty is the plastic surgery operation for correcting defects, deformities, and disfigurations of the eyelids; and for aesthetically modifying the eye region of the face. With the excision and the removal, or the repositioning of excess tissues, such as skin and adipocyte fat, and the reinforcement of the corresponding muscle and tendon tissues, the blepharoplasty procedure resolves functional and cosmetic problems of the periorbita, which is the area from the eyebrow to the upper portion of the cheek. The procedure is more common among women, who accounted for approximately 85% of blepharoplasty procedures in 2014 in the US and 88% of such procedures in the UK.

Gluteoplasty denotes the plastic surgery and the liposuction procedures for the correction of the congenital, traumatic, and acquired defects and deformities of the buttocks and the anatomy of the gluteal region; and for the aesthetic enhancement of the contour of the buttocks.
ICD-9-CM Volume 3 is a system of procedural codes used by health insurers to classify medical procedures for billing purposes. It is a subset of the International Statistical Classification of Diseases and Related Health Problems (ICD) 9-CM. Volumes 1 and 2 are used for diagnostic codes.

Anal fistula is a chronic abnormal communication between the epithelialised surface of the anal canal and usually the perianal skin. An anal fistula can be described as a narrow tunnel with its internal opening in the anal canal and its external opening in the skin near the anus. Anal fistulae commonly occur in people with a history of anal abscesses. They can form when anal abscesses do not heal properly.
Mastopexy is the plastic surgery mammoplasty procedure for raising sagging breasts upon the chest of the woman, by changing and modifying the size, contour, and elevation of the breasts. In a breast-lift surgery to re-establish an aesthetically proportionate bust for the woman, the critical corrective consideration is the tissue viability of the nipple-areola complex (NAC), to ensure the functional sensitivity of the breasts for lactation and breast-feeding.

Stapled hemorrhoidopexy, is a surgical procedure that involves the cutting and removal of Anal Hemorhoidal Vascular Cushion whose function is to help to seal stools and create continence. Procedure also removes abnormally enlarged hemorrhoidal tissue, followed by the repositioning of the remaining hemorrhoidal tissue back to its normal anatomic position. Severe cases of hemorrhoidal prolapse will normally require surgery. Newer surgical procedures include stapled transanal rectal resection (STARR) and procedure for prolapse and hemorrhoids (PPH). Both STARR and PPH are contraindicated in persons with either enterocele or anismus.
"Tubal Reversal," also called "Tubal Sterilization Reversal," or "Tubal Ligation Reversal," or "Microsurgical Tubal Reanastomosis," is a surgical procedure that can restore fertility to women after a tubal ligation. By rejoining the separated segments of the fallopian tube, tubal reversal can give women the chance to become pregnant again. In some cases, however, the separated segments cannot actually be reattached to each other. In some cases the remaining segment of tube needs to be reimplanted into the uterus. In other cases, when the end of the tube has been removed, a procedure called a neofimbrioplasty must be performed to recreate a functional end of the tube which can then act like the missing fimbria and retrieve the egg that has been released during ovulation.
Lateral internal sphincterotomy is an operation performed on the internal anal sphincter muscle for the treatment of chronic anal fissure. The internal anal sphincter is one of two muscles that comprise the anal sphincter which controls the passage of feces. The procedure helps by lowering the resting pressure of the internal anal sphincter, which improves blood supply to the fissure and allows faster healing. The procedure has been shown to be very effective, with 96% of fissures healing at a median of 3 weeks in one trial.
Urethroplasty is the repair of an injury or defect within the walls of the urethra. Trauma, iatrogenic injury and infections are the most common causes of urethral injury/defect requiring repair. Urethroplasty is regarded as the gold standard treatment for urethral strictures and offers better outcomes in terms of recurrence rates than dilatations and urethrotomies. It is probably the only useful modality of treatment for long and complex strictures though recurrence rates are higher for this difficult treatment group.

In humans, the anus is the external opening of the rectum, located inside the intergluteal cleft and separated from the genitals by the perineum. Two sphincters control the exit of feces from the body during an act of defecation, which is the primary function of the anus. These are the internal anal sphincter and the external anal sphincter, which are circular muscles that normally maintain constriction of the orifice and which relaxes as required by normal physiological functioning. The inner sphincter is involuntary and the outer is voluntary. It is located behind the perineum which is located behind the vagina or scrotum.
Transanal hemorrhoidal dearterialization (THD) is a minimally invasive surgical procedure for the treatment of internal hemorrhoids.
In fecal incontinence (FI), surgery may be carried out if conservative measures alone are not sufficient to control symptoms. There are many surgical options described for FI, and they can be considered in 4 general groups.