Health care reform is for the most part governmental policy that affects health care delivery in a given place. Health care reform typically attempts to:

The American Medical Association (AMA) is an American professional association and lobbying group of physicians and medical students. Founded in 1847, it is headquartered in Chicago, Illinois. Membership was 271,660 in 2022.

Bartholomew Thomas Stupak is an American politician and lobbyist. A member of the Democratic Party, Stupak served as the U.S. representative from Michigan's 1st congressional district from 1993 to 2011.
Universal health care is a health care system in which all residents of a particular country or region are assured access to health care. It is generally organized around providing either all residents or only those who cannot afford on their own, with either health services or the means to acquire them, with the end goal of improving health outcomes.

The National Center for Policy Analysis (NCPA) was a non-profit American think tank whose goals were to develop and promote private alternatives to government regulation and control. Topics it addressed include reforms in health care, taxes, Social Security, welfare, education, and environmental regulation.
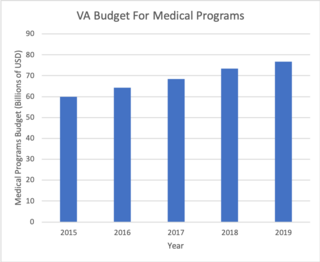
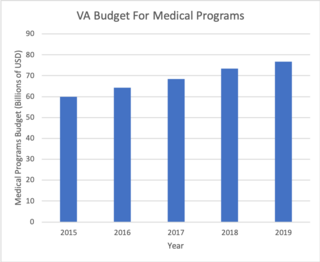
The Veterans Health Administration (VHA) is the component of the United States Department of Veterans Affairs (VA) led by the Under Secretary of Veterans Affairs for Health that implements the healthcare program of the VA through a nationalized healthcare service in the United States, providing healthcare and healthcare-adjacent services to veterans through the administration and operation of 146 VA Medical Centers (VAMC) with integrated outpatient clinics, 772 Community Based Outpatient Clinics (CBOC), and 134 VA Community Living Centers Programs. It is the largest division in the department, and second largest in the entire federal government, employing over 350,000 employees. All VA hospitals, clinics and medical centers are owned by and operated by the Department of Veterans Affairs, and all of the staff employed in VA hospitals are federal employees. Because of this, veterans that qualify for VHA healthcare do not pay premiums or deductibles for their healthcare but may have to make copayments depending on the medical procedure. VHA is not a part of the US Department of Defense Military Health System.
Medical malpractice is professional negligence by act or omission by a health care provider in which the treatment provided falls below the accepted standard of practice in the medical community and causes injury or death to the patient, with most cases involving medical error. Claims of medical malpractice, when pursued in US courts, are processed as civil torts. Sometimes an act of medical malpractice will also constitute a criminal act, as in the case of the death of Michael Jackson.
An urgent care center (UCC), also known as an urgent treatment centre (UTC) in the United Kingdom, is a type of walk-in clinic focused on the delivery of urgent ambulatory care in a dedicated medical facility outside of a traditional emergency department located within a hospital. Urgent care centers primarily treat injuries or illnesses requiring immediate care, but not serious enough to require an ED visit. In the United Kingdom, urgent treatment centres are provided by the National Health Service, which decided in 2019 that all areas of England should be served by a network of urgent treatment centres. In the United States, urgent care centers were first used in the 1970s and have since expanded to approximately 10,000 centers across the country.

John C. Goodman is president and CEO of the Goodman institute for Public Policy Research, a think tank focused on public policy issues. He was the founding chief executive of the National Center for Policy Analysis, which operated from 1982 to 2017. He is a senior fellow at the Independent Institute. The Wall Street Journal and The National Journal have called Goodman the "father of Health Savings Accounts."

Tort reform consists of changes in the civil justice system in common law countries that aim to reduce the ability of plaintiffs to bring tort litigation or to reduce damages they can receive. Such changes are generally justified under the grounds that litigation is an inefficient means to compensate plaintiffs; that tort law permits frivolous or otherwise undesirable litigation to crowd the court system; or that the fear of litigation can serve to curtail innovation, raise the cost of consumer goods or insurance premiums for suppliers of services, and increase legal costs for businesses. Tort reform has primarily been prominent in common law jurisdictions, where criticism of judge-made rules regarding tort actions manifests in calls for statutory reform by the legislature.

Health policy can be defined as the "decisions, plans, and actions that are undertaken to achieve specific healthcare goals within a society". According to the World Health Organization, an explicit health policy can achieve several things: it defines a vision for the future; it outlines priorities and the expected roles of different groups; and it builds consensus and informs people.
David George Gratzer is a physician, columnist, author, Congressional expert witness; he was a senior fellow at both the Manhattan Institute and the Montreal Economic Institute. Though he has written essays on topics as diverse as obesity and political campaigns, he is best known for his first book, published by ECW Press, when he was just 24: Code Blue: Reviving Canada's Health Care System. That book won the Donner Prize established by the Donner Canadian Foundation and was a national bestseller in his native Canada. Gratzer is a critic of the Canadian health care system, and of U.S. President Barack Obama's health care reform proposals. Gratzer was health care policy advisor to Rudy Giuliani's 2008 presidential campaign.
John E. "Jack" Wennberg was the pioneer and leading researcher of unwarranted variation in the healthcare industry. In four decades of work, Wennberg has documented the geographic variation in the healthcare that patients receive in the United States. In 1988, he founded the Center for the Evaluative Clinical Sciences at Dartmouth Medical School to address that unwarranted variation in healthcare.
Healthcare reform in the United States has a long history. Reforms have often been proposed but have rarely been accomplished. In 2010, landmark reform was passed through two federal statutes: the Patient Protection and Affordable Care Act (PPACA), signed March 23, 2010, and the Health Care and Education Reconciliation Act of 2010, which amended the PPACA and became law on March 30, 2010.

Dana Paul Goldman is the dean of the USC Price School of Public Policy, Leonard D. Schaeffer Chair and director of the University of Southern California Leonard D. Schaeffer Center for Health Policy and Economics, and Professor of Public Policy, Pharmacy, and Economics at the Price School and USC School of Pharmacy. He is also an adjunct professor of health services and radiology at UCLA, and a managing director and founding partner, along with Darius Lakdawalla and Tomas J. Philipson, at Precision Heath Economics, a health care consulting firm. Previously held positions include the director of the Bing Center for Health Economics, RAND Royal Center for Health Policy Simulation, and UCLA/RAND Health Services Research Postdoctoral Training Program.
The history of health care reform in the United States has spanned many decades with health care reform having been the subject of political debate since the early part of the 20th century. Recent reforms remain an active political issue. Alternative reform proposals were offered by both of the major candidates in the 2008, 2016, and 2020 presidential elections.
Healthcare rationing in the United States exists in various forms. Access to private health insurance is rationed on price and ability to pay. Those unable to afford a health insurance policy are unable to acquire a private plan except by employer-provided and other job-attached coverage, and insurance companies sometimes pre-screen applicants for pre-existing medical conditions. Applicants with such conditions may be declined cover or pay higher premiums and/or have extra conditions imposed such as a waiting period.

Healthcare in the United States is largely provided by private sector healthcare facilities, and paid for by a combination of public programs, private insurance, and out-of-pocket payments. The U.S. is the only developed country without a system of universal healthcare, and a significant proportion of its population lacks health insurance. The United States spends more on healthcare than any other country, both in absolute terms and as a percentage of GDP; however, this expenditure does not necessarily translate into better overall health outcomes compared to other developed nations. Coverage varies widely across the population, with certain groups, such as the elderly and low-income individuals, receiving more comprehensive care through government programs such as Medicaid and Medicare.
Low-threshold treatment programs are harm reduction-based health care centers targeted towards people who use substances. "Low-threshold" programs are programs that make minimal demands on the patient, offering services without attempting to control their intake of drugs, and providing counselling only if requested. Low-threshold programs may be contrasted with "high-threshold" programs, which require the user to accept a certain level of control and which demand that the patient accept counselling and cease all drug use as a precondition of support.
Black maternal mortality in the United States refers to the death of women, specifically those who identify as Black or African American, during or after child delivery. In general, maternal death can be due to a myriad of factors, such as the nature of the pregnancy or the delivery itself, but is not associated with unintentional or secondary causes. In the United States, around 700 women die from pregnancy-related illnesses or complications per year. This number does not include the approximately 50,000 women who experience life-threatening complications during childbirth, resulting in lifelong disabilities and complications. However, there are stark differences in maternal mortality rates for Black American women versus Indigenous American, Alaska Native, and White American women.