Related Research Articles

Encephalitis is inflammation of the brain. The severity can be variable with symptoms including reduction or alteration in consciousness, headache, fever, confusion, a stiff neck, and vomiting. Complications may include seizures, hallucinations, trouble speaking, memory problems, and problems with hearing.

Bell's palsy is a type of facial paralysis that results in a temporary inability to control the facial muscles on the affected side of the face. In most cases, the weakness is temporary and significantly improves over weeks. Symptoms can vary from mild to severe. They may include muscle twitching, weakness, or total loss of the ability to move one or, in rare cases, both sides of the face. Other symptoms include drooping of the eyebrow, a change in taste, and pain around the ear. Typically symptoms come on over 48 hours. Bell's palsy can trigger an increased sensitivity to sound known as hyperacusis.

Lyme disease, also known as Lyme borreliosis, is a tick-borne disease caused by species of Borrelia bacteria, transmitted by blood-feeding ticks in the genus Ixodes. The most common sign of infection is an expanding red rash, known as erythema migrans (EM), which appears at the site of the tick bite about a week afterwards. The rash is typically neither itchy nor painful. Approximately 70–80% of infected people develop a rash. Early diagnosis can be difficult. Other early symptoms may include fever, headaches and tiredness. If untreated, symptoms may include loss of the ability to move one or both sides of the face, joint pains, severe headaches with neck stiffness or heart palpitations. Months to years later, repeated episodes of joint pain and swelling may occur. Occasionally, shooting pains or tingling in the arms and legs may develop.

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.
Tick-borne diseases, which afflict humans and other animals, are caused by infectious agents transmitted by tick bites. They are caused by infection with a variety of pathogens, including rickettsia and other types of bacteria, viruses, and protozoa. The economic impact of tick-borne diseases is considered to be substantial in humans, and tick-borne diseases are estimated to affect ~80 % of cattle worldwide. Most of these pathogens require passage through vertebrate hosts as part of their life cycle. Tick-borne infections in humans, farm animals, and companion animals are primarily associated with wildlife animal reservoirs. Many tick-borne infections in humans involve a complex cycle between wildlife animal reservoirs and tick vectors. The survival and transmission of these tick-borne viruses are closely linked to their interactions with tick vectors and host cells. These viruses are classified into different families, including Asfarviridae, Reoviridae, Rhabdoviridae, Orthomyxoviridae, Bunyaviridae, and Flaviviridae.
Facial nerve paralysis is a common problem that involves the paralysis of any structures innervated by the facial nerve. The pathway of the facial nerve is long and relatively convoluted, so there are a number of causes that may result in facial nerve paralysis. The most common is Bell's palsy, a disease of unknown cause that may only be diagnosed by exclusion of identifiable serious causes.
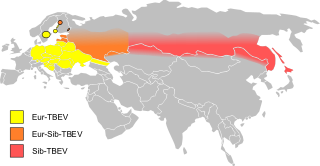
Tick-borne encephalitis (TBE) is a viral infectious disease involving the central nervous system. The disease most often manifests as meningitis, encephalitis or meningoencephalitis. Myelitis and spinal paralysis also occurs. In about one third of cases sequelae, predominantly cognitive dysfunction, persist for a year or more.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.

Meningoencephalitis, also known as herpes meningoencephalitis, is a medical condition that simultaneously resembles both meningitis, which is an infection or inflammation of the meninges, and encephalitis, which is an infection or inflammation of the brain tissue.

Erythema migrans or erythema chronicum migrans is an expanding rash often seen in the early stage of Lyme disease, and can also be caused by southern tick-associated rash illness (STARI). It can appear anywhere from one day to one month after a tick bite. This rash does not represent an allergic reaction to the bite, but rather an actual skin infection of one of the Lyme bacteria species from the genus Borrelia. The rash's name comes from Neo-Latin for "migrating redness."

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.
Neuroborreliosis is a disorder of the central nervous system. A neurological manifestation of Lyme disease, neuroborreliosis is caused by a systemic infection of spirochetes of the genus Borrelia. Symptoms of the disease include erythema migrans and flu-like symptoms.

Human granulocytic anaplasmosis (HGA) is a tick-borne, infectious disease caused by Anaplasma phagocytophilum, an obligate intracellular bacterium that is typically transmitted to humans by ticks of the Ixodes ricinus species complex, including Ixodes scapularis and Ixodes pacificus in North America. These ticks also transmit Lyme disease and other tick-borne diseases.

Mollaret's meningitis is a recurrent or chronic inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. Since Mollaret's meningitis is a recurrent, benign (non-cancerous), aseptic meningitis, it is also referred to as benign recurrent lymphocytic meningitis. It was named for Pierre Mollaret, the French neurologist who first described it in 1944.

Orthostatic headache is a medical condition in which a person develops a headache while vertical and the headache is relieved when horizontal. Previously it was often misdiagnosed as different primary headache disorders such as migraine or tension headaches. Increasing awareness of the symptom and its causes has prevented delayed or missed diagnosis.

A cerebrospinal fluid leak is a medical condition where the cerebrospinal fluid (CSF) that surrounds the brain and spinal cord leaks out of one or more holes or tears in the dura mater. A CSF leak is classed as either spontaneous (primary), having no known cause, or nonspontaneous (secondary) where it is attributed to an underlying condition. Causes of a primary CSF leak are those of trauma including from an accident or intentional injury, or arising from a medical intervention known as iatrogenic. A basilar skull fracture as a cause can give the sign of CSF leakage from the ear, nose or mouth. A lumbar puncture can give the symptom of a post-dural-puncture headache.
The International Lyme and Associated Diseases Society is a non-profit advocacy group which advocates for greater acceptance of the controversial and unrecognized diagnosis "chronic Lyme disease". ILADS was formed by advocates for the recognition of "chronic Lyme disease" including physicians, patients and laboratory personnel, and has published alternative treatment guidelines and diagnostic criteria due to the disagreement with mainstream consensus medical views on Lyme disease.

Lymphocytic pleocytosis is an abnormal increase in the amount of lymphocytes in the cerebrospinal fluid (CSF). It is usually considered to be a sign of infection or inflammation within the nervous system, and is encountered in a number of neurological diseases, such as pseudomigraine, Susac's syndrome, and encephalitis. While lymphocytes make up roughly a quarter of all white blood cells (WBC) in the body, they are generally rare in the CSF. Under normal conditions, there are usually less than 5 white blood cells per μL of CSF. In a pleocytic setting, the number of lymphocytes can jump to more than 1,000 cells per μL. Increases in lymphocyte count are often accompanied by an increase in cerebrospinal protein concentrations in addition to pleocytosis of other types of white blood cells.
Chronic Lyme disease (CLD) is the name used by some people with non-specific symptoms, such as fatigue, muscle pain, and cognitive dysfunction to refer to their condition, even if there is no evidence that they had Lyme disease. Both the label and the belief that these people's symptoms are caused by this particular infection are generally rejected by medical professionals. Chronic Lyme disease is distinct from post-treatment Lyme disease syndrome, a set of lingering symptoms which may persist after successful antibiotic treatment of infection with Lyme-causing Borrelia bacteria, and which may have similar symptoms to those associated with CLD.

Baggio–Yoshinari syndrome, formerly known as the Brazilian Lyme-like disease and Brazilian human borreliosis, is a disease transmitted by the bites of Amblyomma and Rhipicephalus genera ticks, but the organism that causes the infection is a distinct variant of the bacteria that causes Lyme with different markers that cannot be reliably detected by the standard North American tests. Clinical features resemble those of Lyme disease (LD) but have distinctive differences.
References
- ↑ Hindfelt, B.; Jeppsson, P. G.; Nilsson, B.; Olsson, J. E.; Ryberg, B.; Sörnäs, R. (1982-10-01). "Clinical and cerebrospinal fluid findings in lymphocytic meningo-radiculitis (Bannwarth's syndrome)". Acta Neurologica Scandinavica. 66 (4): 444–453. doi: 10.1111/j.1600-0404.1982.tb06866.x . ISSN 0001-6314. PMID 7148387. S2CID 29270560.
- ↑ Ryberg, B. (1984-01-01). "Bannwarth's syndrome (lymphocytic meningoradiculitis) in Sweden". The Yale Journal of Biology and Medicine. 57 (4): 499–503. ISSN 0044-0086. PMC 2590032 . PMID 6516452.
- ↑ Mygland, A (2010). "EFNS guidelines on the diagnosis and management of European Lyme neuroborreliosis". European Journal of Neurology. 17 (1): 8–e4. doi: 10.1111/j.1468-1331.2009.02862.x . PMID 19930447. S2CID 14166137.
- ↑ Rauer, Sebastian; et al. (27 February 2020). "Guidelines for diagnosis and treatment in neurology – Lyme neuroborreliosis". GMS German Medical Science. 18: Doc03. doi:10.3205/000279. PMC 7174852 . PMID 32341686.
- ↑ Lantos, Paul M; et al. (23 January 2021). "Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease". Clinical Infectious Diseases. 72 (1): e1–e48. doi: 10.1093/cid/ciaa1215 . PMID 33417672.
- ↑ Weber, Klaus; Burgdorfer, Willy (2012-12-06). Aspects of Lyme Borreliosis. Springer Science & Business Media. ISBN 9783642776144.