Intensive care medicine, also called critical care medicine, is a medical specialty that deals with seriously or critically ill patients who have, are at risk of, or are recovering from conditions that may be life-threatening. It includes providing life support, invasive monitoring techniques, resuscitation, and end-of-life care. Doctors in this specialty are often called intensive care physicians, critical care physicians or intensivists.

Telenursing refers to the use of information technology in the provision of nursing services whenever physical distance exists between patient and nurse, or between any number of nurses. As a field, it is part of telemedicine, and has many points of contacts with other medical and non-medical applications, such as telediagnosis, teleconsultation, and telemonitoring. The field, however, is still being developed as the information on telenursing isn't comprehensive enough.

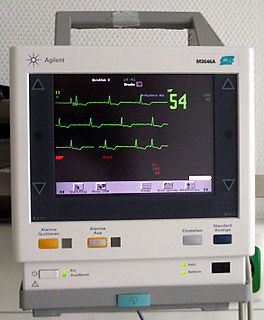
Vital signs are a group of the four to six most important medical signs that indicate the status of the body’s vital (life-sustaining) functions. These measurements are taken to help assess the general physical health of a person, give clues to possible diseases, and show progress toward recovery. The normal ranges for a person’s vital signs vary with age, weight, gender, and overall health.
Nursing assessment is the gathering of information about a patient's physiological, psychological, sociological, and spiritual status by a licensed Registered Nurse. Nursing assessment is the first step in the nursing process. A section of the nursing assessment may be delegated to certified nurses aides. Vitals and EKG's may be delegated to certified nurses aides or nursing techs. It differs from a medical diagnosis. In some instances, the nursing assessment is very broad in scope and in other cases it may focus on one body system or mental health. Nursing assessment is used to identify current and future patient care needs. It incorporates the recognition of normal versus abnormal body physiology. Prompt recognition of pertinent changes along with the skill of critical thinking allows the nurse to identify and prioritize appropriate interventions. An assessment format may already be in place to be used at specific facilities and in specific circumstances.
A post-anesthesia care unit, often abbreviated PACU and sometimes referred to as post-anesthesia recovery or PAR, or simply Recovery, is a vital part of hospitals, ambulatory care centers, and other medical facilities. It is an area, normally attached to operating room suites, designed to provide care for patients recovering from general anesthesia, regional anesthesia, or local anesthesia.

A trauma team is a multidisciplinary group of healthcare workers under the direction of a team leader, who work together to assess and treat the severely injured. This team typically meets before the patient reaches the trauma center. Upon arrival, the team does an initial assessment and necessary resuscitation, adhering to a defined protocol.

An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensive care medicine.
Hospital emergency codes are coded messages often announced over a public address system of a hospital to alert staff to various classes of on-site emergencies. The use of codes is intended to convey essential information quickly and with minimal misunderstanding to staff while preventing stress and panic among visitors to the hospital. Such codes are sometimes posted on placards throughout the hospital or are printed on employee identification badges for ready reference.

Critical care nursing is the field of nursing with a focus on the utmost care of the critically ill or unstable patients following extensive injury, surgery or life threatening diseases. Critical care nurses can be found working in a wide variety of environments and specialties, such as general intensive care units, medical intensive care units, surgical intensive care units, trauma intensive care units, coronary care units, cardiothoracic intensive care units, burns unit, paediatrics and some trauma center emergency departments. These specialists generally take care of critically ill patients who require mechanical ventilation by way of endotracheal intubation and/or titratable vasoactive intravenous medications.

Emergency nursing is a specialty within the field of professional nursing focusing on the care of patients who require prompt medical attention to avoid long-term disability or death. In addition to addressing "true emergencies," emergency nurses increasingly care for people who are unwilling or unable to get primary medical care elsewhere and come to emergency departments for help. In fact, only a small percentage of emergency department (ED) patients have emergency conditions such as a stroke, heart attack or major trauma. Emergency nurses also tend to patients with acute alcohol and/or drug intoxication, psychiatric and behavioral problems and those who have been raped.
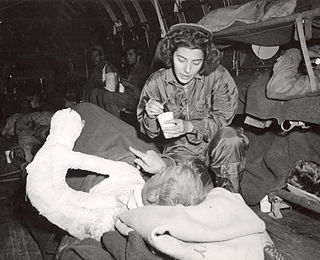
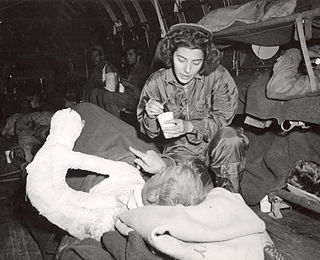
A flight nurse is a registered nurse who specialises in the field of providing comprehensive pre-hospital, emergency critical care, and hospital care to a vast scope of patients. The care of these patients is generally during aeromedical evacuation or rescue operations aboard helicopters, propeller aircraft or jet aircraft. On board a rescue aircraft you would find a flight nurse accompanied by flight medics and respiratory practitioners, as well as the option of a flight physician for comprehensive emergency and critical transport teams. The inclusion of a flight physician is more commonly seen in pediatric and neonatal transport teams. A critical care flight nurse must be able to deal with all age groups with broad critical emergencies. With no physicians on site the nurses scope of practice is expanded. The critical care experience is transferred over to a flight nurse with impacting factors such as altitude and changes in pressure, gravitational forces, and weather. Some patients may experience exacerbation's because of factors related to the cabin environment including hypoxia, limited mobility, gas expansion, and risk of injury related to turbulence and resources with definitive care are limited. Aeromedical evacuation crews coordinate with other organizations to plan for the safe and timely care and evacuation of patients. Crews must be prepared for patients suffering from trauma and mental health illnesses.
An early warning score (EWS) is a guide used by medical services to quickly determine the degree of illness of a patient. It is based on the vital signs. Scores were developed in the late 1990s when studies showed that in-hospital deterioration and cardiac arrest were often preceded by a period of increasing abnormalities in the vital signs.

A pediatric intensive care unit, usually abbreviated to PICU, is an area within a hospital specializing in the care of critically ill infants, children, teenagers, and young adults aged 0-21. A PICU is typically directed by one or more pediatric intensivists or PICU consultants and staffed by doctors, nurses, and respiratory therapists who are specially trained and experienced in pediatric intensive care. The unit may also have nurse practitioners, physician assistants, physiotherapists, social workers, child life specialists, and clerks on staff, although this varies widely depending on geographic location. The ratio of professionals to patients is generally higher than in other areas of the hospital, reflecting the acuity of PICU patients and the risk of life-threatening complications. Complex technology and equipment is often in use, particularly mechanical ventilators and patient monitoring systems. Consequently, PICUs have a larger operating budget than many other departments within the hospital.
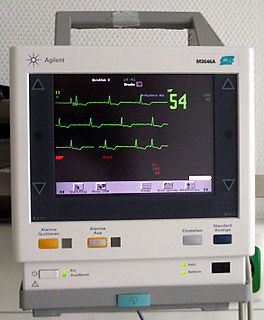
In medicine, monitoring is the observation of a disease, condition or one or several medical parameters over time.

Telehomecare (THC) is a subfield within telehealth. It involves the delivery of healthcare services to patients at home through the use of telecommunications technologies, which enable the interaction of voice, video, and health-related data. The management of care is done from an external site by a healthcare professional.
Vital Sign Alert System is an alert system designed by nurses at Sentara Norfolk General Hospital in Norfolk, Virginia. The alert system, which replaced an ineffective early warning scoring (EWS) system, is a unique creation designed specifically to enhance patient monitoring on medical–surgical and step-down nursing units without increasing the nurse's workload.
A rapid response system (RRS) is a tool implemented in hospitals designed to identify and respond to patients with early signs of clinical deterioration on non-intensive care units with the goal of preventing respiratory or cardiac arrest. A RRS consists of two clinical components and two organizational components.

Believers Church Medical College Hospital (BCMCH) is a healthcare institution of Believers Church based in Thiruvalla, Kerala, India. The Medical College is attached to a 743-bed, multi-speciality hospital. The Medical College, established in 2016, is situated in a campus of about 25 acres (10 ha) connected by rail and road.
Pediatric Early Warning Signs (PEWS) are clinical manifestations that indicate rapid deterioration in pediatric patients, infancy to adolescence. PEWS Score or PEWS System are objective assessment tools that incorporate the clinical manifestations that have the greatest impact on patient outcome.
The impact of the COVID-19 pandemic on hospitals became severe for some hospital systems of the United States in the spring of 2020, a few months after the COVID-19 pandemic began. Some had started to run out of beds, along with having shortages of nurses and doctors. By November 2020, with 13 million cases so far, hospitals throughout the country had been overwhelmed with record numbers of COVID-19 patients. Nursing students had to fill in on an emergency basis, and field hospitals were set up to handle the overflow.