Related Research Articles
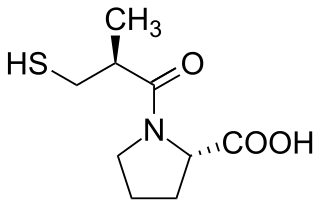
Angiotensin-converting-enzyme inhibitors are a class of medication used primarily for the treatment of high blood pressure and heart failure. This class of medicine works by causing relaxation of blood vessels as well as a decrease in blood volume, which leads to lower blood pressure and decreased oxygen demand from the heart.

Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms itself. It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia. Hypertension is a major cause of premature death worldwide.

Beta blockers, also spelled β-blockers, are a class of medications that are predominantly used to manage abnormal heart rhythms (arrhythmia), and to protect the heart from a second heart attack after a first heart attack. They are also widely used to treat high blood pressure, although they are no longer the first choice for initial treatment of most patients.

Cardiovascular disease (CVD) is any disease involving the heart or blood vessels. CVDs constitute a class of diseases that includes: coronary artery diseases, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, arrhythmia, congenital heart disease, valvular heart disease, carditis, aortic aneurysms, peripheral artery disease, thromboembolic disease, and venous thrombosis.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, angiotensin-converting enzyme inhibitors (ACEis), angiotensin II receptor blockers or antagonists (ARBs), and beta blockers.
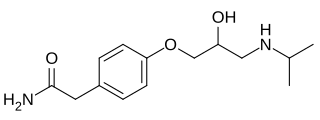
Atenolol is a beta blocker medication primarily used to treat high blood pressure and heart-associated chest pain. Although used to treat high blood pressure, it does not seem to improve mortality in those with the condition. Other uses include the prevention of migraines and treatment of certain irregular heart beats. It is taken orally or by intravenous injection. It can also be used with other blood pressure medications.

Nitrazepam, sold under the brand name Mogadon among others, is a hypnotic drug of the benzodiazepine class used for short-term relief from severe, disabling anxiety and insomnia. It also has sedative (calming) properties, as well as amnestic, anticonvulsant, and skeletal muscle relaxant effects.
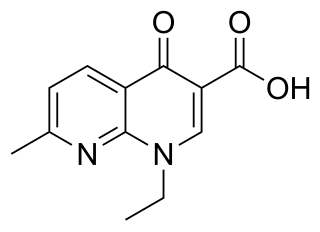
Nalidixic acid is the first of the synthetic quinolone antibiotics.

An adrenergic antagonist is a drug that inhibits the function of adrenergic receptors. There are five adrenergic receptors, which are divided into two groups. The first group of receptors are the beta (β) adrenergic receptors. There are β1, β2, and β3 receptors. The second group contains the alpha (α) adrenoreceptors. There are only α1 and α2 receptors. Adrenergic receptors are located near the heart, kidneys, lungs, and gastrointestinal tract. There are also α-adreno receptors that are located on vascular smooth muscle.
Benoxaprofen, also known as benoxaphen, is a chemical compound with the formula C16H12ClNO3. It is a non-steroidal anti-inflammatory drug (NSAID) of the arylpropionic acid class, and was marketed under the brand name Opren in the United Kingdom and Europe by Eli Lilly and Company (commonly referred to as Lilly), and as Oraflex in the United States of America (USA). Lilly suspended sales of Oraflex in 1982 after reports from the British government and the United States Food and Drug Administration (US FDA) of adverse effects and deaths linked to the drug.

Ciclazindol (WY-23409) is an antidepressant and anorectic drug of the tetracyclic chemical class that was developed in the mid to late 1970s, but was never marketed. It acts as a norepinephrine reuptake inhibitor, and to a lesser extent as a dopamine reuptake inhibitor. Ciclazindol has no effects on the SERT, 5-HT receptors, mACh receptors, or α-adrenergic receptors, and has only weak affinity for the H1 receptor. As suggested by its local anesthetic properties, ciclazindol may also inhibit sodium channels. It is known to block potassium channels as well.
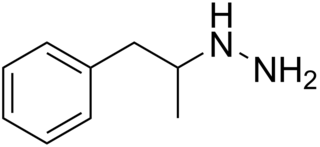
Pheniprazine, formerly sold under the brand names Catron and Cavodil, is an irreversible and non-selective monoamine oxidase inhibitor (MAOI) of the hydrazine group that was used as an antidepressant to treat depression in the 1960s. It was also used in the treatment of angina pectoris and schizophrenia. Pheniprazine has been largely discontinued due to toxicity concerns such as jaundice, amblyopia, and optic neuritis.

Mepiprazole is an anxiolytic drug of the phenylpiperazine group with additional antidepressant properties that is marketed in Spain. It acts as a 5-HT2A and α1-adrenergic receptor antagonist and inhibits the reuptake and induces the release of serotonin, dopamine, and norepinephrine to varying extents, and has been described as a serotonin antagonist and reuptake inhibitor (SARI). Controlled clinical trials of mepiprazole in patients with irritable bowel syndrome (IBS) were also carried out and suggested some benefits of the drug in relieving symptoms of IBS in some patients. Similarly to other phenylpiperazines like trazodone, nefazodone, and etoperidone, mepiprazole produces mCPP as an active metabolite.

Tiamenidine (BAN, USAN, INN, also known as thiamenidine, Hoe 440) is an imidazoline compound that shares many of the pharmacological properties of clonidine. It is a centrally-acting α2 adrenergic receptor agonist (IC50 = 9.1 nM). It also acts as an α1-adrenergic receptor agonist to a far lesser extent (IC50 = 4.85 μM). In hypertensive volunteers, like clonidine, it significantly increased sinus node recovery time and lowered cardiac output. It was marketed (as tiamenidine hydrochloride) by Sanofi-Aventis under the brand name Sundralen for the management of essential hypertension.
Renal sympathetic denervation (RSDN) is a minimally invasive, endovascular catheter based procedure using radiofrequency ablation or ultrasound ablation aimed at treating resistant hypertension. Nerves in the wall of the renal artery are ablated by applying radiofrequency pulses or ultrasound to the renal arteries. This causes reduction of sympathetic afferent and efferent activity to the kidney and blood pressure can be decreased. Early data from international clinical trials without sham controls was promising - demonstrating large blood pressure reductions in patients with treatment-resistant hypertension. However, in 2014 a prospective, single-blind, randomized, sham-controlled clinical trial failed to confirm a beneficial effect on blood pressure. A 2014 consensus statement from The Joint UK Societies did not recommend the use of renal denervation for treatment of resistant hypertension on current evidence. More recent sham-controlled trials suggest renal denervation can lead to lower systolic blood pressure.
Joseph Gavin Collier is a British retired clinical pharmacologist and emeritus professor of medicines policy at St George's Hospital and Medical School in London, whose early research included establishing the effect of aspirin on human prostaglandins and looking at the role of nitric oxide and angiotensin converting enzyme in controlling blood vessel tone and blood pressure. Later, in his national policy work, he helped change the way drugs are priced and bought by the NHS, and ensured that members of governmental advisory committees published their conflicts of interest.
John Douglas Swales (1935–2000) was an English cardiologist, professor of medicine, medical journal editor, and internationally recognised expert on hypertension.
Malcolm Davenport Milne (1915–1991) was an English physician and nephrologist.
Non-pharmacological intervention (NPI) is any type of healthcare intervention which is not primarily based on medication. Some examples include exercise, sleep improvement, and dietary habits.
Emma Harriet Baker is a British professor of clinical pharmacology and consultant physician in internal medicine at St George's Hospital, London. She has a specialist interest in people who have multiple medical conditions at the same time and take several medications, with a particular focus on lung disease. She is director of the UK's first BSc in clinical pharmacology, clinical vice president of the British Pharmacological Society and training programme director at Health Education England.
References
- ↑ Janes, Cath (6 August 2009). "A controversial career". Careers. BMJ: b3072. doi:10.1136/bmj.b3072. S2CID 79577367.
- 1 2 Stuart R. Walker, ed. (1993). Quality of life assessment : key issues in 1990s. Dordrecht u.a.: Kluwer. pp. xv–xvi. ISBN 978-0-7923-8991-0.
- ↑ "The Pharma Letter".
- 1 2 "Death of Sean Rigg" (PDF). IPCC. Archived from the original (PDF) on 24 August 2012. Retrieved 5 December 2012.
- ↑ "Man disabled by MMR vaccine awarded £90,000 after 13-year fight". The Telegraph. Archived from the original on 31 August 2010.
- ↑ "Newer antidepressants for the treatment of depression in ad". The BMJ. 17 November 2018.
- ↑ "Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis". The BMJ. 17 November 2018.
- ↑ "Report by The Prisoner Ombudsman into the circumstances surrounding the death of Aaron Hogg" (PDF). Northern Ireland Prisoner Ombudsman.
- ↑ "Report by The Prisoner Ombudsman into the circumstances surrounding the death of Frances McKeown" (PDF). Northern Ireland Prisoner Ombudsman.
- ↑ "Sedative at centre of Jackson probe". Daily Express.
- ↑ "Sedative at centre of Michael Jackson 'homicide' probe". The London Evening Standard.