A disease is a particular abnormal condition that adversely affects the structure or function of all or part of an organism and is not immediately due to any external injury. Diseases are often known to be medical conditions that are associated with specific signs and symptoms. A disease may be caused by external factors such as pathogens or by internal dysfunctions. For example, internal dysfunctions of the immune system can produce a variety of different diseases, including various forms of immunodeficiency, hypersensitivity, allergies, and autoimmune disorders.

Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.

An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance. The emergency department is usually found in a hospital or other primary care center.
Medical privacy, or health privacy, is the practice of maintaining the security and confidentiality of patient records. It involves both the conversational discretion of health care providers and the security of medical records. The terms can also refer to the physical privacy of patients from other patients and providers while in a medical facility, and to modesty in medical settings. Modern concerns include the degree of disclosure to insurance companies, employers, and other third parties. The advent of electronic medical records (EMR) and patient care management systems (PCMS) have raised new concerns about privacy, balanced with efforts to reduce duplication of services and medical errors.

The Health Insurance Portability and Accountability Act of 1996 is a United States Act of Congress enacted by the 104th United States Congress and signed into law by President Bill Clinton on August 21, 1996. It aimed to alter the transfer of healthcare information, stipulated the guidelines by which personally identifiable information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and addressed some limitations on healthcare insurance coverage. It generally prohibits healthcare providers and businesses called covered entities from disclosing protected information to anyone other than a patient and the patient's authorized representatives without their consent. The bill does not restrict patients from receiving information about themselves. Furthermore, it does not prohibit patients from voluntarily sharing their health information however they choose, nor does it require confidentiality where a patient discloses medical information to family members, friends or other individuals not employees of a covered entity.
Prognosis is a medical term for predicting the likelihood or expected development of a disease, including whether the signs and symptoms will improve or worsen or remain stable over time; expectations of quality of life, such as the ability to carry out daily activities; the potential for complications and associated health issues; and the likelihood of survival. A prognosis is made on the basis of the normal course of the diagnosed disease, the individual's physical and mental condition, the available treatments, and additional factors. A complete prognosis includes the expected duration, function, and description of the course of the disease, such as progressive decline, intermittent crisis, or sudden, unpredictable crisis.

The terms medical record, health record and medical chart are used somewhat interchangeably to describe the systematic documentation of a single patient's medical history and care across time within one particular health care provider's jurisdiction. A medical record includes a variety of types of "notes" entered over time by healthcare professionals, recording observations and administration of drugs and therapies, orders for the administration of drugs and therapies, test results, X-rays, reports, etc. The maintenance of complete and accurate medical records is a requirement of health care providers and is generally enforced as a licensing or certification prerequisite.

Family medicine is a medical specialty within primary care that provides continuing and comprehensive health care for the individual and family across all ages, genders, diseases, and parts of the body. The specialist, who is usually a primary care physician, is named a family physician. It is often referred to as general practice and a practitioner as a general practitioner. Historically, their role was once performed by any doctor with qualifications from a medical school and who works in the community. However, since the 1950s, family medicine / general practice has become a specialty in its own right, with specific training requirements tailored to each country. The names of the specialty emphasize its holistic nature and/or its roots in the family. It is based on knowledge of the patient in the context of the family and the community, focusing on disease prevention and health promotion. According to the World Organization of Family Doctors (WONCA), the aim of family medicine is "promoting personal, comprehensive and continuing care for the individual in the context of the family and the community". The issues of values underlying this practice are usually known as primary care ethics.

Vital signs are a group of the four to six most crucial medical signs that indicate the status of the body's vital (life-sustaining) functions. These measurements are taken to help assess the general physical health of a person, give clues to possible diseases, and show progress toward recovery. The normal ranges for a person's vital signs vary with age, weight, sex, and overall health.

Emergency psychiatry is the clinical application of psychiatry in emergency settings. Conditions requiring psychiatric interventions may include attempted suicide, substance abuse, depression, psychosis, violence or other rapid changes in behavior.
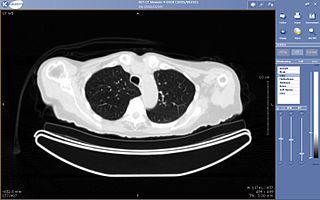
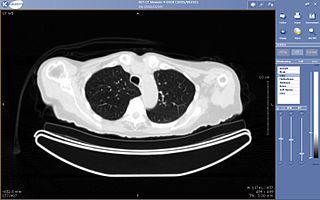
Teleradiology is the transmission of radiological patient images from procedures such as x-rays photographs, Computed tomography (CT), and MRI imaging, from one location to another for the purposes of sharing studies with other radiologists and physicians. Teleradiology allows radiologists to provide services without actually having to be at the location of the patient. This is particularly important when a sub-specialist such as an MRI radiologist, neuroradiologist, pediatric radiologist, or musculoskeletal radiologist is needed, since these professionals are generally only located in large metropolitan areas working during daytime hours. Teleradiology allows for specialists to be available at all times.

A trauma team is a multidisciplinary group of healthcare workers under the direction of a team leader that works together to assess and treat the severely injured. This team typically meets before the patient reaches the trauma center. Upon arrival, the team does an initial assessment and necessary resuscitation, adhering to a defined protocol.
In the healthcare industry, pay for performance (P4P), also known as "value-based purchasing", is a payment model that offers financial incentives to physicians, hospitals, medical groups, and other healthcare providers for meeting certain performance measures. Clinical outcomes, such as longer survival, are difficult to measure, so pay for performance systems usually evaluate process quality and efficiency, such as measuring blood pressure, lowering blood pressure, or counseling patients to stop smoking. This model also penalizes health care providers for poor outcomes, medical errors, or increased costs. Integrated delivery systems where insurers and providers share in the cost are intended to help align incentives for value-based care.
A virtual ward allows patients to get the care they need at home safely and conveniently, rather than being in hospital.

The South Central Ambulance Service NHS Foundation Trust (SCAS) is the ambulance service for the counties of Berkshire, Buckinghamshire, Oxfordshire and most of Hampshire. It is a foundation trust of the National Health Service, and one of ten NHS ambulance trusts in England. As of August 2022, SCAS is currently rated Inadequate by the CQC following multiple failings within the trust. SCAS is the only Ambulance Service in England to have received this rating.

The East of England Ambulance Service NHS Trust (EEAST) is an NHS trust responsible for providing National Health Service (NHS) ambulance services in the counties of Bedfordshire, Cambridgeshire, Essex, Hertfordshire, Norfolk and Suffolk, in the East of England region. These consist of approximately 6.2 million people across an area of 7,500 square miles (19,000 km2).

An early warning system (EWS), sometimes called a between-the-flags or track-and-trigger chart, is a clinical tool used in healthcare to anticipate patient deterioration by measuring the cumulative variation in observations, most often being patient vital signs and level of consciousness. EWSs emerged in the 1990s with research finding deterioration was often preceded by abnormal vital signs. Early warning systems are heavily utilised internationally with some jurisdictions mandating their use.

The National Health Service (NHS) is the publicly funded healthcare system in England, and one of the four National Health Service systems in the United Kingdom. It is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde. Primarily funded by the government from general taxation, and overseen by the Department of Health and Social Care, the NHS provides healthcare to all legal English residents and residents from other regions of the UK, with most services free at the point of use for most people. The NHS also conducts research through the National Institute for Health and Care Research (NIHR).
Healthcare in England is mainly provided by the National Health Service (NHS), a public body that provides healthcare to all permanent residents in England, that is free at the point of use. The body is one of four forming the UK National Health Service, as health is a devolved matter; there are differences with the provisions for healthcare elsewhere in the United Kingdom, and in England it is overseen by NHS England. Though the public system dominates healthcare provision in England, private health care and a wide variety of alternative and complementary treatments are available for those willing and able to pay.

Medical diagnosis is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as a diagnosis with the medical context being implicit. The information required for a diagnosis is typically collected from a history and physical examination of the person seeking medical care. Often, one or more diagnostic procedures, such as medical tests, are also done during the process. Sometimes the posthumous diagnosis is considered a kind of medical diagnosis.