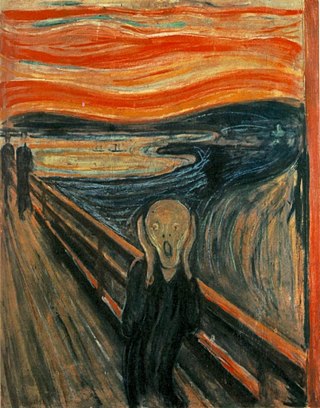
Anxiety is an emotion which is characterised by an unpleasant state of inner turmoil and includes feelings of dread over anticipated events. Anxiety is different from fear in that fear is defined as the emotional response to a present threat, whereas anxiety is the anticipation of a future one. It is often accompanied by nervous behavior such as pacing back and forth, somatic complaints, and rumination.

Cognitive behavioral therapy (CBT) is a form of psychotherapy that aims to reduce symptoms of various mental health conditions, primarily depression, PTSD and anxiety disorders. Cognitive behavioral therapy focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include many issues and the treatment of many mental health and other conditions, including anxiety, substance use disorders, marital problems, ADHD, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.
A mental disorder, also referred to as a mental illness, a mental health condition, or a psychiatric disability, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. A mental disorder is also characterized by a clinically significant disturbance in an individual's cognition, emotional regulation, or behavior, often in a social context. Such disturbances may occur as single episodes, may be persistent, or may be relapsing–remitting. There are many different types of mental disorders, with signs and symptoms that vary widely between specific disorders. A mental disorder is one aspect of mental health.
Anxiety disorders are a group of mental disorders characterized by significant and uncontrollable feelings of anxiety and fear such that a person's social, occupational, and personal functions are significantly impaired. Anxiety may cause physical and cognitive symptoms, such as restlessness, irritability, easy fatigue, difficulty concentrating, increased heart rate, chest pain, abdominal pain, and a variety of other symptoms that may vary based on the individual.
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that develops from experiencing a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life or well-being. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event. Young children are less likely to show distress, but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.

Hypochondriasis or hypochondria is a condition in which a person is excessively and unduly worried about having a serious illness. Hypochondria is an old concept whose meaning has repeatedly changed over its lifespan. It has been claimed that this debilitating condition results from an inaccurate perception of the condition of body or mind despite the absence of an actual medical diagnosis. An individual with hypochondriasis is known as a hypochondriac. Hypochondriacs become unduly alarmed about any physical or psychological symptoms they detect, no matter how minor the symptom may be, and are convinced that they have, or are about to be diagnosed with, a serious illness.
Generalized anxiety disorder (GAD) is a mental and behavioral disorder, specifically an anxiety disorder characterized by excessive, uncontrollable and often irrational worry about events or activities. Worry often interferes with daily functioning, and individuals with GAD are often overly concerned about everyday matters such as health, finances, death, family, relationship concerns, or work difficulties. Symptoms may include excessive worry, restlessness, trouble sleeping, exhaustion, irritability, sweating, and trembling.
Adjustment disorder is a maladaptive response to a psychosocial stressor. It is classified as a mental disorder. The maladaptive response usually involves otherwise normal emotional and behavioral reactions that manifest more intensely than usual, causing marked distress, preoccupation with the stressor and its consequences, and functional impairment.

Mental health encompasses emotional, psychological, and social well-being, influencing cognition, perception, and behavior. According to World Health Organization (WHO), it is a "state of well-being in which the individual realizes his or her abilities, can cope with the normal stresses of life, can work productively and fruitfully, and can contribute to his or her community". It likewise determines how an individual handles stress, interpersonal relationships, and decision-making. Mental health includes subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one's intellectual and emotional potential, among others. From the perspectives of positive psychology or holism, mental health may include an individual's ability to enjoy life and to create a balance between life activities and efforts to achieve psychological resilience. Cultural differences, personal philosophy, subjective assessments, and competing professional theories all affect how one defines "mental health". Some early signs related to mental health difficulties are sleep irritation, lack of energy, lack of appetite, thinking of harming oneself or others, self-isolating, and frequently zoning out.

College health is a desired outcome created by a constellation of services, programs and policies directed at advancing the health and wellbeing of individuals enrolled in an institution of higher education, while also addressing and improving both population health and community health. Many colleges and universities worldwide apply both health promotion and health care as processes to achieve key performance indicators in college health. The variety of healthcare services provided by any one institution range from first aid stations employing a single nurse to large, accredited, multi-specialty ambulatory healthcare clinics with hundreds of employees. These services, programs and policies require a multidisciplinary team, the healthcare services alone include physicians, physician assistants, administrators, nurses, nurse practitioners, mental health professionals, health educators, athletic trainers, dietitians and nutritionists, and pharmacists. Some of the healthcare services extend to include massage therapists and other holistic health care professionals. While currently changing, the vast majority of college health services are set up as cost centers or service units rather than as parts of academic departments or health care delivery enterprises.
Mixed anxiety–depressive disorder (MADD) is a diagnostic category that defines patients who have both anxiety and depressive symptoms of limited and equal intensity accompanied by at least some autonomic nervous system features. Autonomic features are involuntary physical symptoms usually caused by an overactive nervous system, such as panic attacks or intestinal distress. The World Health Organization's ICD-10 describes Mixed anxiety and depressive disorder: "...when symptoms of anxiety and depression are both present, but neither is clearly predominant, and neither type of symptom is present to the extent that justifies a diagnosis if considered separately. When both anxiety and depressive symptoms are present and severe enough to justify individual diagnoses, both diagnoses should be recorded and this category should not be used."
Improving Access to Psychological Therapies (IAPT), also known as NHS Talking Therapies, for anxiety and depression, is a National Health Service initiative to provide more psychotherapy to the general population in England. It was developed and introduced by the Labour Party as a result of economic evaluations by Professor Lord Richard Layard, based on new therapy guidelines from the National Institute for Health and Care Excellence as promoted by clinical psychologist David M. Clark.
Metacognitive therapy (MCT) is a psychotherapy focused on modifying metacognitive beliefs that perpetuate states of worry, rumination and attention fixation. It was created by Adrian Wells based on an information processing model by Wells and Gerald Matthews. It is supported by scientific evidence from a large number of studies.

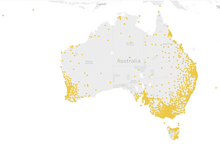
Richard Allan Bryant is an Australian medical scientist. He is Scientia Professor of Psychology at the University of New South Wales (UNSW) and director of the UNSW Traumatic Stress Clinic, based at UNSW and Westmead Institute for Medical Research. His main areas of research are posttraumatic stress disorder (PTSD) and prolonged grief disorder. On 13 June 2016 he was appointed a Companion of the Order of Australia (AC), for eminent service to medical research in the field of psychotraumatology, as a psychologist and author, to the study of Indigenous mental health, as an advisor to a range of government and international organisations, and to professional societies.
Operational stress injury or OSI is a non-clinical, non-medical term referring to a persistent psychological difficulty caused by traumatic experiences or prolonged high stress or fatigue during service as a military member or first responder. The term does not replace any individual diagnoses or disorders, but rather describes a category of mental health concerns linked to the particular challenges that these military members or first responders encounter in their service. There is not yet a single fixed definition. The term was first conceptualized within the Canadian Armed Forces to help foster understanding of the broader mental health challenges faced by military members who have been impacted by traumatic experiences and who face difficulty as a result. OSI encompasses a number of the diagnoses found in the Diagnostic and Statistical Manual of Mental Disorders (DSM) classification system, with the common thread being a linkage to the operational experiences of the afflicted. The term has gained traction outside of the military community as an appropriate way to describe similar challenges suffered by those whose work regularly exposes them to trauma, particularly front line emergency first responders such as but not limited to police, firefighters, paramedics, correctional officers, and emergency dispatchers. The term, at present mostly used within Canada, is increasingly significant in the development of legislation, policy, treatments and benefits in the military and first responder communities.
The nine-item Patient Health Questionnaire (PHQ-9) is a depressive symptom scale and diagnostic tool introduced in 2001 to screen adult patients in primary care settings. The instrument assesses for the presence and severity of depressive symptoms and a possible depressive disorder. The PHQ-9 is a component of the larger self-administered Patient Health Questionnaire (PHQ), but can be used as a stand-alone instrument. The PHQ is part of Pfizer's larger suite of trademarked products, called the Primary Care Evaluation of Mental Disorders (PRIME-MD). The PHQ-9 takes less than three minutes to complete. It is scored by simply adding up the individual items' scores. Each of the nine items reflects a DSM-5 symptom of depression. Primary care providers can use the PHQ-9 to screen for possible depression in patients.

Michelle G. Craske is an Australian academic who is currently serving as Professor of Psychology, Psychiatry, and Behavioral Sciences, Miller Endowed Chair, Director of the Anxiety and Depression Research Center, and Associate Director of the Staglin Family Music Center for Behavioral and Brain Health at the University of California, Los Angeles. She is known for her research on anxiety disorders, including phobia and panic disorder, and the use of fear extinction through exposure therapy as treatment. Other research focuses on anxiety and depression in childhood and adolescence and the use of cognitive behavioral therapy as treatment. Craske has served as President of the Association for Behavioral and Cognitive Therapy. She was a member of the DSM-IV work group on Anxiety Disorders and the DSM-5 work group on Anxiety, Obsessive Compulsive Spectrum, Posttraumatic, and Dissociative Disorders, while chairing the sub-work group on Anxiety Disorders. She is the Editor-in-chief of Behaviour Research and Therapy.
Paternal depression is a psychological disorder derived from parental depression. Paternal depression affects the mood of men; fathers and caregivers in particular. 'Father' may refer to the biological father, foster parent, social parent, step-parent or simply the carer of the child. This mood disorder exhibits symptoms similar to postpartum depression (PPD) including anxiety, insomnia, irritability, consistent breakdown and crying episodes, and low energy. This may negatively impact family relationships and the upbringing of children. Parents diagnosed with parental depression often experience increased stress and anxiety levels during early pregnancy, labor and postpartum. Those with parental depression may have developed it early on but some are diagnosed later on from when the child is a toddler up until a young adult.
Anne Marie Albano is a clinical psychologist known for her clinical work and research on psychosocial treatments for anxiety and mood disorders, and the impact of these disorders on the developing youth. She is the CUCARD professor of medical psychology in psychiatry at Columbia University, the founding director of the Columbia University Clinic for Anxiety and Related Disorders (CUCARD), and the clinical site director at CUCARD of the New York Presbyterian Hospital's Youth Anxiety Center.

Internet-based treatments for trauma survivors is a growing class of online treatments that allow for an individual who has experienced trauma to seek and receive treatment without needing to attend psychotherapy in person. The progressive movement to online resources and the need for more accessible mental health services has given rise to the creation of online-based interventions aimed to help those who have experienced traumatic events. Cognitive behavioral therapy (CBT) has shown to be particularly effective in the treatment of trauma-related disorders and adapting CBT to an online format has been shown to be as effective as in-person CBT in the treatment of trauma. Due to its positive outcomes, CBT-based internet treatment options for trauma survivors has been an expanding field in both research and clinical settings.