Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid used medically to treat chronic pain and opioid use disorder. Prescribed for daily use, the medicine relieves cravings and opioid withdrawal symptoms. Withdrawal management using methadone can be accomplished in less than a month, or it may be done gradually over a longer period of time, or simply maintained for the rest of the patient's life. While a single dose has a rapid effect, maximum effect can take up to five days of use. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.
Chronic pain or chronic pain syndrome is a type of pain that is also known by other titles such as gradual burning pain, electrical pain, throbbing pain, and nauseating pain. This type of pain is sometimes confused with acute pain and can last from three months to several years; various diagnostic manuals such as DSM-5 and ICD-11 have proposed several definitions of chronic pain, but the accepted definition is that it is "pain that lasts longer than the expected period of recovery."

Pain management is an aspect of medicine and health care involving relief of pain in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals provide some pain control in the normal course of their practice, and for the more complex instances of pain, they also call on additional help from a specific medical specialty devoted to pain, which is called pain medicine.
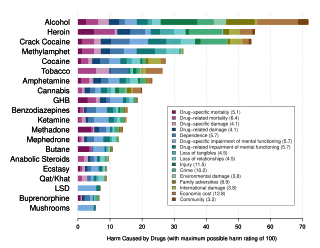
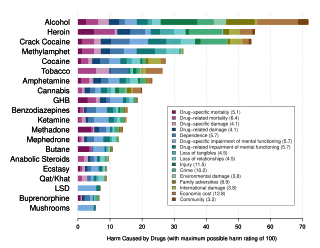
Drug rehabilitation is the process of medical or psychotherapeutic treatment for dependency on psychoactive substances such as alcohol, prescription drugs, and street drugs such as cannabis, cocaine, heroin, and amphetamines. The general intent is to enable the patient to confront substance dependence, if present, and stop substance misuse to avoid the psychological, legal, financial, social, and medical consequences that can be caused.
Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids. Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are important components of opioid use disorder.

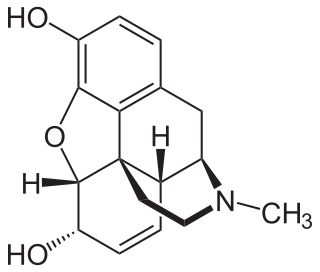
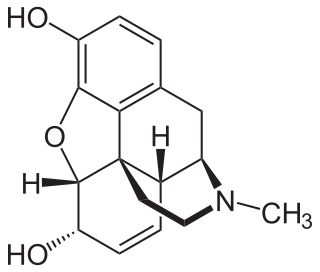
Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, the patient must have moderate opioid withdrawal symptoms before buprenorphine can be administered under direct observation of a health-care provider.
In internal medicine, relapse or recidivism is a recurrence of a past condition. For example, multiple sclerosis and malaria often exhibit peaks of activity and sometimes very long periods of dormancy, followed by relapse or recrudescence.
Substance dependence, also known as drug dependence, is a biopsychological situation whereby an individual's functionality is dependent on the necessitated re-consumption of a psychoactive substance because of an adaptive state that has developed within the individual from psychoactive substance consumption that results in the experience of withdrawal and that necessitates the re-consumption of the drug. A drug addiction, a distinct concept from substance dependence, is defined as compulsive, out-of-control drug use, despite negative consequences. An addictive drug is a drug which is both rewarding and reinforcing. ΔFosB, a gene transcription factor, is now known to be a critical component and common factor in the development of virtually all forms of behavioral and drug addictions, but not dependence.
Attentional bias refers to how a person's perception is affected by selective factors in their attention. Attentional biases may explain an individual's failure to consider alternative possibilities when occupied with an existing train of thought. For example, cigarette smokers have been shown to possess an attentional bias for smoking-related cues around them, due to their brain's altered reward sensitivity. Attentional bias has also been associated with clinically relevant symptoms such as anxiety and depression.
Cue reactivity is a type of learned response which is observed in individuals with an addiction and involves significant physiological and psychological reactions to presentations of drug-related stimuli. The central tenet of cue reactivity is that cues previously predicting receipt of drug reward under certain conditions can evoke stimulus associated responses such as urges to use drugs. In other words, learned cues can signal drug reward, in that cues previously associated with drug use can elicit cue-reactivity such as arousal, anticipation, and changes in behavioral motivation. Responses to a drug cue can be physiological, behavioral, or symbolic expressive. The clinical utility of cue reactivity is based on the conceptualization that drug cues elicit craving which is a critical factor in the maintenance and relapse to drug use. Additionally, cue reactivity allows for the development of testable hypotheses grounded in established theories of human behavior. Therefore, researchers have leveraged the cue reactivity paradigm to study addiction, antecedents of relapse, and craving, translate pre-clinical findings to clinical samples, and contribute to the development of new treatment methods. Testing cue reactivity in human samples involves exposing individuals with a substance use disorder to drug-related cues and drug neutral cues, and then measuring their reactions by assessing changes in self-reported drug craving and physiological responses.
Low-dose naltrexone (LDN) refers to daily naltrexone dosages that are roughly one-tenth of the standard opioid addiction treatment dosage. Most published research suggests a daily dosage of 4.5 mg, but this can vary by a few milligrams. Low-dose naltrexone has been studied for the treatment of multiple chronic pain disorders including fibromyalgia, multiple sclerosis, Crohn’s disease, and complex regional pain syndrome.
An addictive behavior is a behavior, or a stimulus related to a behavior, that is both rewarding and reinforcing, and is associated with the development of an addiction. There are two main forms of addiction: substance use disorders and behavioral addiction. The parallels and distinctions between behavioral addictions and other compulsive behavior disorders like bulimia nervosa and obsessive-compulsive disorder (OCD) are still being researched by behavioral scientists.

The psychological and physiological effects of meditation have been studied. In recent years, studies of meditation have increasingly involved the use of modern instruments, such as functional magnetic resonance imaging and electroencephalography, which are able to observe brain physiology and neural activity in living subjects, either during the act of meditation itself or before and after meditation. Correlations can thus be established between meditative practices and brain structure or function.
Management of ME/CFS focuses on symptoms management, as no treatments that address the root cause of the illness are available. Pacing, or regulating one's activities to avoid triggering worse symptoms, is the most common management strategy for post-exertional malaise. Clinical management varies widely, with many patients receiving combinations of therapies. The prognosis of ME/CFS is poor, with recovery considered “rare”.
Mindfulness-Based Stress Reduction (MBSR) therapy is a mindfulness-based program (MBP) designed for stress management and used to treat other conditions. It is structured as an eight to ten week group program.
Euphoric recall is a cognitive bias that describes the tendency of people to remember past experiences in a positive light, while overlooking negative experiences associated with some event(s). Euphoric recall has primarily been cited as a factor in substance dependence. Individuals may become obsessed with recreating the remembered pleasures of the past, where positive expectancy of outcomes results in the belief that substance use can provide immediate relief.
Cognitive behavioral training (CBTraining), sometimes referred to as structured cognitive behavioral training, (SCBT) is an organized process that uses systematic, highly-structured tasks designed to improve cognitive functions. Functions such as working memory, decision making, and attention are thought to inform whether a person defaults to an impulsive behavior or a premeditated behavior. The aim of CBTraining is to affect a person's decision-making process and cause them to choose the premeditated behavior over the impulsive behavior in their everyday life. Through scheduled trainings that may be up to a few hours long and may be weekly or daily over a specific set of time, the goal of CBTraining is to show that focusing on repetitive, increasingly difficult cognitive tasks can transfer those skills to other cognitive processes in your brain, leading to behavioral change. There has been a recent resurgence of interest in this field with the invention of new technologies and a greater understanding of cognition in general.

The opioid epidemic, also referred to as the opioid crisis, is the rapid increase in the overuse, misuse/abuse, and overdose deaths attributed either in part or in whole to the class of drugs called opiates/opioids since the 1990s. It includes the significant medical, social, psychological, demographic and economic consequences of the medical, non-medical, and recreational abuse of these medications.
Opioid agonist therapy (OAT) is a treatment in which prescribed opioid agonists are given to patients who live with Opioid use disorder (OUD). In the case of methadone maintenance treatment (MMT), methadone is used to treat dependence on heroin or other opioids, and is administered on an ongoing basis.

Prescription drug addiction is the chronic, repeated use of a prescription drug in ways other than prescribed for, including using someone else’s prescription. A prescription drug is a pharmaceutical drug that may not be dispensed without a legal medical prescription. Drugs in this category are supervised due to their potential for misuse and substance use disorder. The classes of medications most commonly abused are opioids, central nervous system (CNS) depressants and central nervous stimulants. In particular, prescription opioid is most commonly abused in the form of prescription analgesics.