Scoliosis is a condition in which a person's spine has an irregular curve in the coronal plane. The curve is usually S- or C-shaped over three dimensions. In some, the degree of curve is stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, but more severe cases can affect breathing and movement. Pain is usually present in adults, and can worsen with age. As the condition progresses, it may alter a person's life, and hence can also be considered a disability. It can be compared to kyphosis and lordosis, other abnormal curvatures of the spine which are in the sagittal plane (front-back) rather than the coronal (left-right).

Kyphosis is an abnormally excessive convex curvature of the spine as it occurs in the thoracic and sacral regions. Abnormal inward concave lordotic curving of the cervical and lumbar regions of the spine is called lordosis.

A discectomy is the surgical removal of abnormal disc material that presses on a nerve root or the spinal cord. The procedure involves removing a portion of an intervertebral disc, which causes pain, weakness or numbness by stressing the spinal cord or radiating nerves. The traditional open discectomy, or Love's technique, was published by Ross and Love in 1971. Advances have produced visualization improvements to traditional discectomy procedures, or endoscopic discectomy. In conjunction with the traditional discectomy or microdiscectomy, a laminotomy is often involved to permit access to the intervertebral disc. Laminotomy means a significant amount of typically normal bone is removed from the vertebra, allowing the surgeon to better see and access the area of disc herniation.

A laminectomy is a surgical procedure that removes a portion of a vertebra called the lamina, which is the roof of the spinal canal. It is a major spine operation with residual scar tissue and may result in postlaminectomy syndrome. Depending on the problem, more conservative treatments may be viable.

Degenerative disc disease (DDD) is a medical condition typically brought on by the aging process in which there are anatomic changes and possibly a loss of function of one or more intervertebral discs of the spine. DDD can take place with or without symptoms, but is typically identified once symptoms arise. The root cause is thought to be loss of soluble proteins within the fluid contained in the disc with resultant reduction of the oncotic pressure, which in turn causes loss of fluid volume. Normal downward forces cause the affected disc to lose height, and the distance between vertebrae is reduced. The anulus fibrosus, the tough outer layers of a disc, also weakens. This loss of height causes laxity of the longitudinal ligaments, which may allow anterior, posterior, or lateral shifting of the vertebral bodies, causing facet joint malalignment and arthritis; scoliosis; cervical hyperlordosis; thoracic hyperkyphosis; lumbar hyperlordosis; narrowing of the space available for the spinal tract within the vertebra ; or narrowing of the space through which a spinal nerve exits with resultant inflammation and impingement of a spinal nerve, causing a radiculopathy.

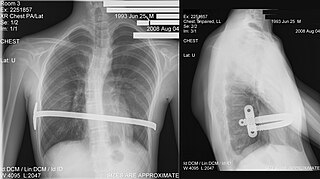
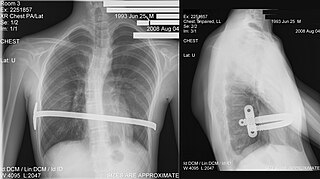
The Harrington rod is a stainless steel surgical device. Historically, this rod was implanted along the spinal column to treat, among other conditions, a lateral or coronal-plane curvature of the spine, or scoliosis. Up to one million people had Harrington rods implanted for scoliosis between the early 1960s and the late 1990s.

A back brace is a device designed to limit the motion of the spine in cases of bone fracture or in post-operative spinal fusiona, as well as a preventative measure against some progressive conditions or to correct a patient's posture.

Spinal fusion, also called spondylodesis or spondylosyndesis, is a surgery performed by orthopaedic surgeons or neurosurgeons that joins two or more vertebrae. This procedure can be performed at any level in the spine and prevents any movement between the fused vertebrae. There are many types of spinal fusion and each technique involves using bone grafting—either from the patient (autograft), donor (allograft), or artificial bone substitutes—to help the bones heal together. Additional hardware is often used to hold the bones in place while the graft fuses the two vertebrae together. The placement of hardware can be guided by fluoroscopy, navigation systems, or robotics.
The Nuss procedure is a minimally invasive procedure, invented in 1987 by Dr. Donald Nuss and his colleagues, Dr. Daniel Croitoru and Dr. Robert Kelly, for treating pectus excavatum. He developed it at Children's Hospital of The King's Daughters, in Norfolk, Virginia. The operation typically takes approximately two hours.

Kyphoscoliosis describes an abnormal curvature of the spine in both the coronal and sagittal planes. It is a combination of kyphosis and scoliosis. This musculoskeletal disorder often leads to other issues in patients, such as under-ventilation of lungs, pulmonary hypertension, difficulty in performing day-to-day activities, and psychological issues emanating from anxiety about acceptance among peers, especially in young patients. It can also be seen in syringomyelia, Friedreich's ataxia, spina bifida, kyphoscoliotic Ehlers–Danlos syndrome (kEDS), and Duchenne muscular dystrophy due to asymmetric weakening of the paraspinal muscles.

Scheuermann's disease is a skeletal disorder. It describes a condition where the vertebrae grow unevenly with respect to the sagittal plane; that is, the posterior angle is often greater than the anterior. This uneven growth results in the signature "wedging" shape of the vertebrae, causing kyphosis. It is named after Danish surgeon Holger Scheuermann.

Anterior cervical discectomy and fusion (ACDF) is a surgical procedure to treat nerve root or spinal cord compression by decompressing the spinal cord and nerve roots of the cervical spine with a discectomy, followed by inter-vertebral fusion to stabilize the corresponding vertebrae. This procedure is used when other non-surgical treatments have failed.
Lobectomy of the lung is a surgical operation where a lobe of the lung is removed. It is done to remove a portion of diseased lung, such as early stage lung cancer.

A laminotomy is an orthopaedic neurosurgical procedure that removes part of the lamina of a vertebral arch in order to relieve pressure in the vertebral canal. A laminotomy is less invasive than conventional vertebral column surgery techniques, such as laminectomy because it leaves more ligaments and muscles attached to the spinous process intact and it requires removing less bone from the vertebra. As a result, laminotomies typically have a faster recovery time and result in fewer postoperative complications. Nevertheless, possible risks can occur during or after the procedure like infection, hematomas, and dural tears. Laminotomies are commonly performed as treatment for lumbar spinal stenosis and herniated disks. MRI and CT scans are often used pre- and post surgery to determine if the procedure was successful.

Spinal disease refers to a condition impairing the backbone. These include various diseases of the back or spine ("dorso-"), such as kyphosis. Dorsalgia refers to back pain. Some other spinal diseases include spinal muscular atrophy, ankylosing spondylitis, scoliosis, lumbar spinal stenosis, spina bifida, spinal tumors, osteoporosis and cauda equina syndrome.

Lumbar provocative discography is an invasive diagnostic procedure for evaluation for intervertebral disc pathology. It is usually reserved for persons with persistent, severe low back pain (LBP) who have abnormal spaces between vertebrae on magnetic resonance imaging (MRI), where other diagnostic tests have failed to reveal clear confirmation of a suspected disc as the source of pain, and surgical intervention is being considered.
Minimally invasive spine surgery, also known as MISS, has no specific meaning or definition. It implies a lack of severe surgical invasion. The older style of open-spine surgery for a relatively small disc problem used to require a 5-6 inch incision and a month in the hospital. MISS techniques utilize more modern technology, advanced imaging techniques and special medical equipment to reduce tissue trauma, bleeding, radiation exposure, infection risk, and decreased hospital stays by minimizing the size of the incision. Modern endoscopic procedures can be done through a 2 to 5 mm skin opening. By contrast, procedures done with a microscope require skin openings of approximately one inch, or more.
The sacroiliac joint is a paired joint in the pelvis that lies between the sacrum and an ilium. Due to its location in the lower back, a dysfunctional sacroiliac joint may cause lower back and/or leg pain. The resulting leg pain can be severe, resembling sciatica or a slipped disc. While nonsurgical treatments are effective for some, others have found that surgery for the dysfunctional sacroiliac joint is the only method to relieve pain.
The management of scoliosis is complex and is determined primarily by the type of scoliosis encountered: syndromic, congenital, neuromuscular, or idiopathic. Treatment options for idiopathic scoliosis are determined in part by the severity of the curvature and skeletal maturity, which together help predict the likelihood of progression. Non-surgical treatment should be pro-active with intervention performed early as "Best results were obtained in 10-25 degrees scoliosis which is a good indication to start therapy before more structural changes within the spine establish." Treatment options have historically been categorized under the following types:
- Observation
- Bracing
- Specialized physical therapy
- Surgery
Anterior vertebral body tethering (AVBT) is a relatively new surgery for the treatment of scoliosis in pediatric patients. Left untreated, severe scoliosis can worsen and eventually affect a person's lungs and heart.