Modesty in medical settings refers to the practices and equipment used to preserve patient modesty in medical examination and clinics.
Modesty in medical settings refers to the practices and equipment used to preserve patient modesty in medical examination and clinics.
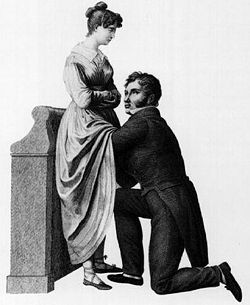
Prior to the invention of the stethoscope, a physician who wanted to perform auscultation to listen to heart sounds or noise inside a body would have to physically place their ear against the body of the person being examined. [1] In 1816, male physician René Laennec invented the stethoscope as a way to respect the modesty of a female patient, as it would have been awkward for him to put his ear on her chest. [1]
Hospital gowns increase modesty as compared to the patient presenting nude, but in the past, there have been odd clothing which exposes the body. [2] Some contemporary changes to the design of hospital gowns have been proposed. [2]
The American Urological Association recommends that all children receive genital and anorectal examinations at routine physical examinations. Pediatric male genital examinations prioritize checking for capability of foreskin retraction and testicular abnormalities. Pediatric female genital examinations involve inspecting for swelling of the labia, imperforate hymen, and vaginal discharge. Both male and female pediatric genital and anorectal examinations also check for urethral discharge, hernias, hydroceles, and defects of the spinal cord and spinal column.
During pediatric genital and anorectal exams, communication techniques should be tailored to the developmental level of the child. Providers should ask for permission at each step of the examination, explain the process, and clearly communicate with parents and caregivers who are present. Older children should have the opportunity to have a non-parental chaperone. [3]
In places with more cultural diversity, people from minority groups often make specific requests for modesty in healthcare; some minority women consequently do not access healthcare. [4] [5] Muslims in non-Muslim societies also occasionally make requests for modesty. [6] [7]