Related Research Articles

Interstitial cystitis (IC), a type of bladder pain syndrome (BPS), is chronic pain that affects the bladder and pelvic floor. Together with Chronic prostatitis/chronic pelvic pain syndrome, it makes up urologic chronic pelvic pain syndrome (UCPPS). Symptoms include feeling the need to urinate right away, needing to urinate often, and pain with sex. IC/BPS is associated with depression and lower quality of life. Many of those affected also have irritable bowel syndrome and fibromyalgia.

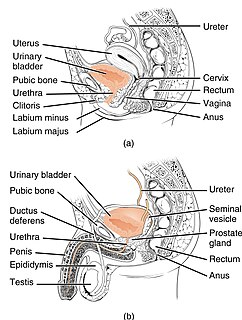
Urology, also known as genitourinary surgery, is the branch of medicine that focuses on surgical and medical diseases of the male and female urinary-tract system and the male reproductive organs. Organs under the domain of urology include the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs.
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis.

Fecal incontinence (FI), or in some forms encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits, and receptive anal sex. An estimated 2.2% of community dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.

Kegel exercise, also known as pelvic-floor exercise, involves repeatedly contracting and relaxing the muscles that form part of the pelvic floor, now sometimes colloquially referred to as the "Kegel muscles". The exercise can be performed many times a day, for several minutes at a time but takes one to three months to begin to have an effect.
Arnold Henry Kegel was an American gynecologist who invented the Kegel perineometer and Kegel exercises as non-surgical treatment of urinary incontinence from perineal muscle weakness and/or laxity. Today pelvic floor exercises are widely held as first-line treatment for urinary stress incontinence and any type of female incontinence and female genital prolapse, with evidence supporting its use from systematic reviews of randomized trials in the Cochrane Library amongst others. Kegel first published his ideas in 1948. He was Assistant Professor of Gynecology at the Keck School of Medicine of USC.

A pessary is a prosthetic device inserted into the vagina for structural and pharmaceutical purposes. It is most commonly used to treat stress urinary incontinence to stop urinary leakage, and pelvic organ prolapse to maintain the location of organs in the pelvic region. It can also be used to administer medications locally in the vagina or as a method of contraception. Pessaries come in different shapes and sizes, so it is important that individuals be fitted for them by health care professionals to avoid any complications. However, there are a few instances and circumstances that allow individuals to purchase pessaries from a store without a prescription or without seeking help from a health care professional. Some side effects may occur if pessaries are not sized properly or regularly maintained, but with the appropriate care, pessaries are generally safe and well tolerated.

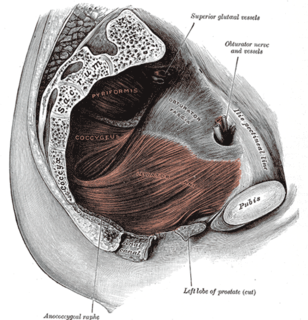
The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region below. Both males and females have a pelvic floor. To accommodate the birth canal, a female's pelvic cavity is larger than a male's.

Pelvic floor dysfunction is a term used for a variety of disorders that occur when pelvic floor muscles and ligaments are impaired. The condition affects up to 50 percent of women who have given birth. Although this condition predominantly affects women, up to 16 percent of men suffer as well. Symptoms can include pelvic pain, pressure, pain during sex, urinary incontinence (UI), overactive bladder, bowel incontinence, incomplete emptying of feces, constipation, myofascial pelvic pain and pelvic organ prolapse. When pelvic organ prolapse occurs, there may be visible organ protrusion or a lump felt in the vagina or anus.

A cystocele, also known as a prolapsed bladder, is a medical condition in which a woman's bladder bulges into her vagina. Some may have no symptoms. Others may have trouble starting urination, urinary incontinence, or frequent urination. Complications may include recurrent urinary tract infections and urinary retention. Cystocele and a prolapsed urethra often occur together and is called a cystourethrocele. Cystocele can negatively affect quality of life.
Pelvic organ prolapse (POP) is characterized by descent of pelvic organs from their normal positions. In women, the condition usually occurs when the pelvic floor collapses after gynecological cancer treatment, childbirth or heavy lifting.
Stress incontinence, also known as stress urinary incontinence (SUI) or effort incontinence is a form of urinary incontinence. It is due to inadequate closure of the bladder outlet by the urethral sphincter.
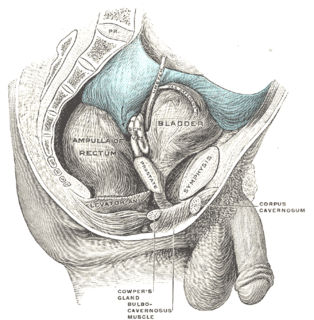
Retropubic space is a potential avascular space located between the pubic symphysis and the urinary bladder. The retropubic space is a preperitoneal space, located behind the transversalis fascia and in front of peritoneum.

Overactive bladder (OAB) is a condition where there is a frequent feeling of needing to urinate to a degree that it negatively affects a person's life. The frequent need to urinate may occur during the day, at night, or both. If there is loss of bladder control then it is known as urge incontinence. More than 40% of people with overactive bladder have incontinence. Conversely, about 40% to 70% of urinary incontinence is due to overactive bladder. Overactive bladder is not life-threatening, but most people with the condition have problems for years.

The urethral sphincters are two muscles used to control the exit of urine in the urinary bladder through the urethra. The two muscles are either the male or female external urethral sphincter and the internal urethral sphincter. When either of these muscles contracts, the urethra is sealed shut.
Urogynecology or urogynaecology is a surgical sub-specialty of urology and gynecology.

Urodynamic testing or urodynamics is a study that assesses how the bladder and urethra are performing their job of storing and releasing urine. Urodynamic tests can help explain symptoms such as:

Overflow incontinence is a form of urinary incontinence, characterized by the involuntary release of urine from an overfull urinary bladder, often in the absence of any urge to urinate. This condition occurs in people who have a blockage of the bladder outlet, or when the muscle that expels urine from the bladder is too weak to empty the bladder normally. Overflow incontinence may also be a side effect of certain medications.
Jerry Blaivas is an American urologist and senior faculty at the Icahn School of Medicine at Mount Sinai in New York City and adjunct professor of Urology at SUNY Downstate Medical School in Brooklyn, as well as professor of clinical urology at College of Physicians and Surgeons, Columbia University and clinical professor of Urology at Weill Medical College of Cornell University. He has four patents pending; received four research grants for which he served as the principal investigator; as of 2018 published 216 peer-reviewed articles, 14 books and 219 book chapters and served as a major in the United States Army assigned to the Walson Army Hospital. He served as president, Urodynamic Society.
Pelvic floor physical therapy (PFPT) is a specialty area within physical therapy focusing on the rehabilitation of muscles in the pelvic floor after injury or dysfunction. It can be used to address issues such as muscle weakness or tightness post childbirth, dyspareunia, vaginismus, vulvodynia, constipation, fecal or urinary incontinence, pelvic organ prolapse, and sexual dysfunction. Licensed physical therapists with specialized pelvic floor physical therapy training address dysfunction in individuals across the gender and sex spectra, though PFPT often associated with women's health for its heavy focus on addressing issues of pelvic trauma after childbirth.
References
- 1 2 3 Kaplan, Rebekah (2016). Clinical Guidelines for Advanced Practice Nursing. Jones & Bartlett Publishers. p. 244. ISBN 978-1-284-09313-1.
- ↑ "National Association for Continence - Company Profile and News". Bloomberg.com. Retrieved 31 December 2020.
- ↑ "Home | Incontinence, Nocturia, Enlarged Prostate, and Prolapse Information". Nafc.org. 2011-09-18. Archived from the original on 2016-05-04. Retrieved 2011-10-29.
- ↑ "National Association For Continence – healthfinder.gov – NAFC". healthfinder.gov. 2011-05-31. Retrieved 2011-10-29.
- 1 2 "National Association for Continence". NORD (National Organization for Rare Disorders). Retrieved 29 December 2020.
- ↑ "National Association For Continence Publishes 14th Edition of its Resource Guide". ICS. Retrieved 30 December 2020.