Related Research Articles

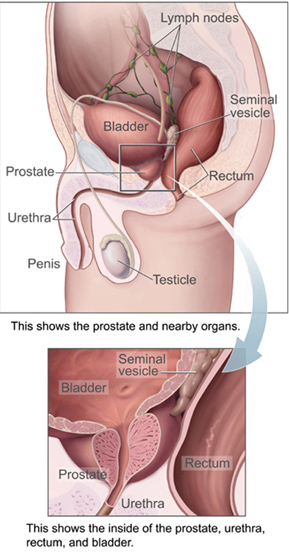
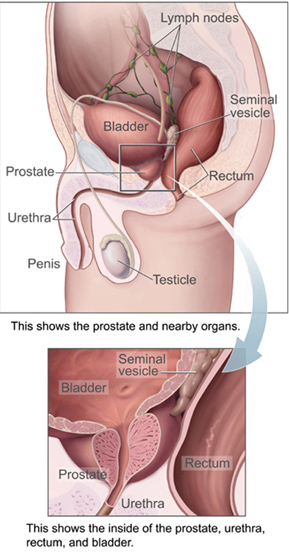
The prostate is both an accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found in all male mammals. It differs between species anatomically, chemically, and physiologically. Anatomically, the prostate is found below the bladder, with the urethra passing through it. It is described in gross anatomy as consisting of lobes and in microanatomy by zone. It is surrounded by an elastic, fibromuscular capsule and contains glandular tissue, as well as connective tissue.

Prostate cancer is the uncontrolled growth of cells in the prostate, a gland in the male reproductive system below the bladder. Abnormal growth of prostate tissue is usually detected through screening tests, typically blood tests that check for prostate-specific antigen (PSA) levels. Those with high levels of PSA in their blood are at increased risk for developing prostate cancer. Diagnosis requires a biopsy of the prostate. If cancer is present, the pathologist assigns a Gleason score, and a higher score represents a more dangerous tumor. Medical imaging is performed to look for cancer that has spread outside the prostate. Based on the Gleason score, PSA levels, and imaging results, a cancer case is assigned a stage 1 to 4. A higher stage signifies a more advanced, more dangerous disease.

Prostatectomy is the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.

Radical retropubic prostatectomy is a surgical procedure in which the prostate gland is removed through an incision in the abdomen. It is most often used to treat individuals who have early prostate cancer. Radical retropubic prostatectomy can be performed under general, spinal, or epidural anesthesia and requires blood transfusion less than one-fifth of the time. Radical retropubic prostatectomy is associated with complications such as urinary incontinence and impotence, but these outcomes are related to a combination of individual patient anatomy, surgical technique, and the experience and skill of the surgeon.
Radical perineal prostatectomy is a surgical procedure wherein the entire prostate gland is removed through an incision in the area between the anus and the scrotum (perineum).
Retroperitoneal lymph node dissection (RPLND) is a surgical procedure to remove abdominal lymph nodes. It is used to treat testicular cancer, as well as to help establish the exact stage and type of the cancer.
The cavernous nerves are post-ganglionic parasympathetic nerves that facilitate penile erection and clitoral erection. They arise from cell bodies in the inferior hypogastric plexus where they receive the pre-ganglionic pelvic splanchnic nerves (S2-S4).
A neurovascular bundle is a structure that binds nerves and veins with connective tissue so that they travel in tandem through the body.
Biochemical recurrence is a rise in the blood level of prostate-specific antigen (PSA) in prostate cancer patients after treatment with surgery or radiation. Biochemical recurrence may occur in patients who do not have symptoms. It may mean that the cancer has come back. Also called PSA failure and biochemical relapse.
Laparoscopic radical prostatectomy (LRP) is a form of radical prostatectomy, an operation for prostate cancer. Contrasted with the original open form of the surgery, it does not make a large incision but instead uses fiber optics and miniaturization.

Brachytherapy is a type of radiotherapy, or radiation treatment, offered to certain cancer patients. There are two types of brachytherapy – high dose-rate (HDR) and low dose-rate (LDR). LDR brachytherapy is the one most commonly used to treat prostate cancer. It may be referred to as 'seed implantation' or it may be called 'pinhole surgery'.

Ashutosh K. Tewari is the chairman of urology at the Icahn School of Medicine at Mount Sinai Hospital in New York City. He is a board certified American urologist, oncologist, and principal investigator. Before moving to the Icahn School of Medicine in 2013, he was the founding director of both the Center for Prostate Cancer at Weill Cornell Medical College and the LeFrak Center for Robotic Surgery at NewYork–Presbyterian Hospital. Dr. Tewari was the Ronald P. Lynch endowed Chair of Urologic Oncology and the hospital's Director of Robotic Prostatectomy, treating patients with prostate, urinary bladder and other urological cancers. He is the current President of the Society for Urologic Robotic Surgeons (SURS) and the Committee Chair of the Prostate Program. Dr. Tewari is a world leading urological surgeon, and has performed over 10,000 robotically assisted procedures using the da Vinci Surgical System. Academically, he is recognized as a world-renowned expert on urologic oncology with over 250 peer reviewed published papers to his credit; he is on such lists as America's Top Doctors, New York Magazine's Best Doctors, and Who's Who in the World. In 2012, he was given the American Urological Association Gold Cystoscope Award for "outstanding contributions to the field of urologic oncology, most notably the treatment of prostate cancer and the development of novel techniques to improve the outcomes of robotic prostatectomy."
Treatment for prostate cancer may involve active surveillance, surgery, radiation therapy – including brachytherapy and external-beam radiation therapy, proton therapy, high-intensity focused ultrasound (HIFU), cryosurgery, hormonal therapy, chemotherapy, or some combination. Treatments also extend to survivorship based interventions. These interventions are focused on five domains including: physical symptoms, psychological symptoms, surveillance, health promotion and care coordination. However, a published review has found only high levels of evidence for interventions that target physical and psychological symptom management and health promotion, with no reviews of interventions for either care coordination or surveillance. The favored treatment option depends on the stage of the disease, the Gleason score, and the PSA level. Other important factors include the man's age, his general health, and his feelings about potential treatments and their possible side-effects. Because all treatments can have significant side-effects, such as erectile dysfunction and urinary incontinence, treatment discussions often focus on balancing the goals of therapy with the risks of lifestyle alterations.

Orchiectomy is a surgical procedure in which one or both testicles are removed. The surgery can be performed for various reasons:

Roger Sinclair Kirby FRCS(Urol), FEBU is a British retired prostate surgeon and professor of urology. He is prominent as a writer on men's health and prostate disease, the founding editor of the journal Prostate Cancer and Prostatic Diseases and Trends in Urology and Men's Health and a fundraiser for prostate disease charities, best known for his use of the da Vinci surgical robot for laparoscopic prostatectomy in the treatment of prostate cancer. He is a co-founder and president of the charity The Urology Foundation (TUF), vice-president of the charity Prostate Cancer UK, trustee of the King Edward VII's Hospital, and from 2020 to 2024 was president of the Royal Society of Medicine (RSM), London.

Michael D. Stifelman Michael D. Stifelman, M.D., is Chair of Urology at Hackensack University Medical Center, Director of Robotic Surgery at Hackensack Meridian Health, and Professor and Inaugural Chair of Urology at Hackensack Meridian School of Medicine.

A parotidectomy is the surgical excision (removal) of the parotid gland, the major and largest of the salivary glands. The procedure is most typically performed due to neoplasms (tumors), which are growths of rapidly and abnormally dividing cells. Neoplasms can be benign (non-cancerous) or malignant (cancerous). The majority of parotid gland tumors are benign, however 20% of parotid tumors are found to be malignant. Parotidectomy is performed mostly by oral and maxillofacial surgeon and ENT surgeon.

Vipul R. Patel, FACS is the founder and Medical Director of the AdventHealth’s Global Robotics Institute, founder and Vice President of the Society of Robotic Surgery, and founder and Editor Emeritus of The Journal of Robotic Surgery. He is board certified by the American Urological Association and specializes in robotic surgery for prostate cancer. On April 29, 2024, Dr. Vipul Patel completed his 18,000th robotic-assisted prostatectomy. The large volume of prostatectomies he has performed has enabled him to amass a large amount of statistical evidence regarding the efficacy of robotic techniques which has been used in developing and refining techniques. Patel credits the use of robotic assisted surgery with helping surgeons achieve better surgical outcomes with the "trifecta" of cancer control, continence and sexual function. In the course of his career Patel has led and participated in studies that have resulted in developing improved outcomes for robotic surgery and urologic treatment.

If medical treatment is not effective, surgery may need to be performed for benign prostatic hyperplasia.
Anthony James Costello, FRACS, FRCSI, is an Australian urologist. He served as head of the department of urology at the Royal Melbourne Hospital, Australia. He established the first robotic prostate cancer surgery programme in Australia and published the first series of men who had laser surgery for benign prostate enlargements.
References
- ↑ "NCI Dictionary of Cancer Terms". National Cancer Institute. 2011-02-02. Retrieved 2020-05-05.
- ↑ Publishing, Harvard Health (9 March 2014). "Prostate cancer surgery: Is nerve-sparing safe?". Harvard Health. Retrieved 2020-05-05.
- ↑ Krishnan, R.; Katz, D.; Nelson, C. J.; Mulhall, J. P. (2014). "Erectile function recovery in patients after non-nerve sparing radical prostatectomy". Andrology. 2 (6): 951–954. doi: 10.1111/andr.282 . ISSN 2047-2927. PMID 25270277.
![]() This article incorporates public domain material from Dictionary of Cancer Terms. U.S. National Cancer Institute.
This article incorporates public domain material from Dictionary of Cancer Terms. U.S. National Cancer Institute.