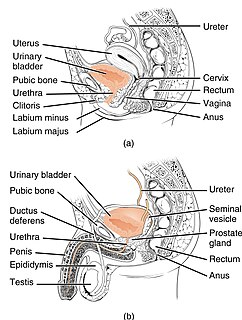
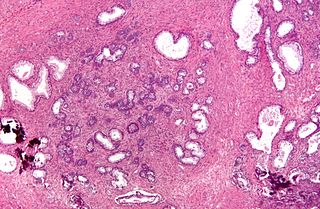
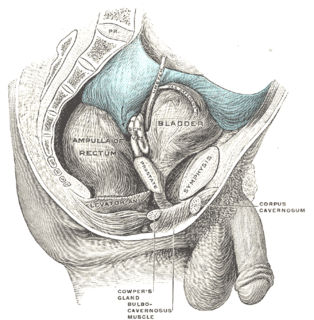
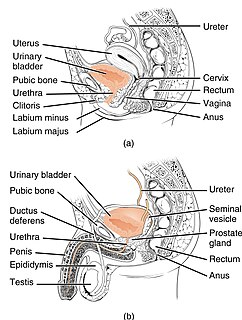
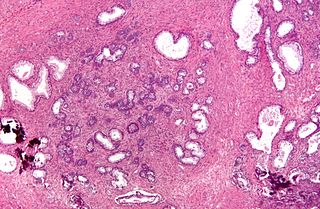
The prostate is both an accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found only in some mammals. It differs between species anatomically, chemically, and physiologically. Anatomically, the prostate is found below the bladder, with the urethra passing through it. It is described in gross anatomy as consisting of lobes and in microanatomy by zone. It is surrounded by an elastic, fibromuscular capsule and contains glandular tissue as well as connective tissue.
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.
Transurethral resection of the prostate is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, it is performed by visualising the prostate through the urethra and removing tissue by electrocautery or sharp dissection. It has been the standard treatment for BPH for many years, but recently alternative, minimally invasive techniques have become available. This procedure is done with spinal or general anaesthetic. A triple lumen catheter is inserted through the urethra to irrigate and drain the bladder after the surgical procedure is complete. Outcome is considered excellent for 80–90% of BPH patients. The procedure carries minimal risk for erectile dysfunction, moderate risk for bleeding, and a large risk for retrograde ejaculation.

Cystectomy is a medical term for surgical removal of all or part of the urinary bladder. It may also be rarely used to refer to the removal of a cyst. The most common condition warranting removal of the urinary bladder is bladder cancer.

Prostatectomy as a medical term refers to the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.

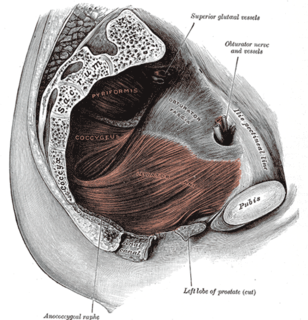
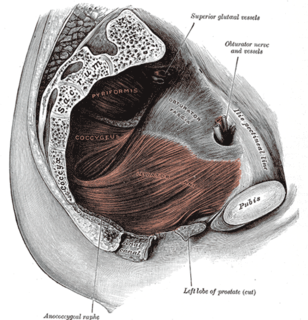
Radical perineal prostatectomy is a surgical procedure wherein the entire prostate gland is removed through an incision in the area between the anus and the scrotum (perineum).
Stress incontinence, also known as stress urinary incontinence (SUI) or effort incontinence is a form of urinary incontinence. It is due to inadequate closure of the bladder outlet by the urethral sphincter.
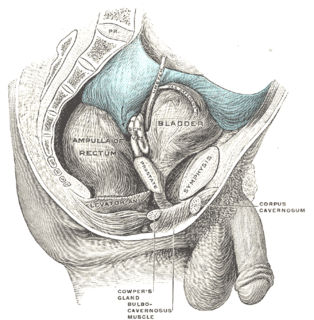
Retropubic space is a potential avascular space located between the pubic symphysis and the urinary bladder. The retropubic space is a preperitoneal space, located behind the transversalis fascia and in front of peritoneum.

The urethral sphincters are two muscles used to control the exit of urine in the urinary bladder through the urethra. The two muscles are either the male or female external urethral sphincter and the internal urethral sphincter. When either of these muscles contracts, the urethra is sealed shut.

Laparoscopic radical prostatectomy (LRP) is a form of radical prostatectomy, an operation for prostate cancer. Contrasted with the original open form of the surgery, it does not make a large incision but instead uses fiber optics and miniaturization.
Nerve-sparing surgery is a type of surgery that attempts to save the nerves near the tissues being removed.

A prostatic stent is a stent used to keep open the male urethra and allow the passing of urine in cases of prostatic obstruction and lower urinary tract symptoms (LUTS). Prostatic obstruction is a common condition with a variety of causes. Benign prostatic hyperplasia (BPH) is the most common cause, but obstruction may also occur acutely after treatment for BPH such as transurethral needle ablation of the prostate (TUNA), transurethral resection of the prostate (TURP), transurethral microwave thermotherapy (TUMT), prostate cancer or after radiation therapy.

Brachytherapy is a type of radiotherapy, or radiation treatment, offered to certain cancer patients. There are two types of brachytherapy – high dose-rate (HDR) and low dose-rate (LDR). LDR brachytherapy is the one most commonly used to treat prostate cancer. It may be referred to as 'seed implantation' or it may be called 'pinhole surgery'.

Ashutosh K. Tewari is the chairman of urology at the Icahn School of Medicine at Mount Sinai Hospital in New York City. He is a board certified American urologist, oncologist, and principal investigator. Before moving to the Icahn School of Medicine in 2013, he was the founding director of both the Center for Prostate Cancer at Weill Cornell Medical College and the LeFrak Center for Robotic Surgery at NewYork–Presbyterian Hospital. Dr. Tewari was the Ronald P. Lynch endowed Chair of Urologic Oncology and the hospital's Director of Robotic Prostatectomy, treating patients with prostate, urinary bladder and other urological cancers. He is the current President of the Society for Urologic Robotic Surgeons (SURS) and the Committee Chair of the Prostate Program. Dr. Tewari is a world leading urological surgeon, and has performed over 9,000 robotically assisted procedures using the da Vinci Surgical System. Academically, he is recognized as a world-renowned expert on urologic oncology with over 250 peer reviewed published papers to his credit; he is on such lists as America's Top Doctors, New York Magazine's Best Doctors, and Who's Who in the World. In 2012, he was given the American Urological Association Gold Cystoscope Award for "outstanding contributions to the field of urologic oncology, most notably the treatment of prostate cancer and the development of novel techniques to improve the outcomes of robotic prostatectomy."
Treatment for prostate cancer may involve active surveillance, surgery, radiation therapy – including brachytherapy and external-beam radiation therapy, proton therapy, high-intensity focused ultrasound (HIFU), cryosurgery, hormonal therapy, chemotherapy, or some combination. Treatments also extend to survivorship based interventions. These interventions are focused on five domains including: physical symptoms, psychological symptoms, surveillance, health promotion and care coordination. However, a published review has found only high levels of evidence for interventions that target physical and psychological symptom management and health promotion, with no reviews of interventions for either care coordination or surveillance. The favored treatment option depends on the stage of the disease, the Gleason score, and the PSA level. Other important factors include the man's age, his general health, and his feelings about potential treatments and their possible side-effects. Because all treatments can have significant side-effects, such as erectile dysfunction and urinary incontinence, treatment discussions often focus on balancing the goals of therapy with the risks of lifestyle alterations.
Mark S. Soloway is a leading authority in urologic cancer, researcher, former departmental Chair, medical professor and invitational lecturer. He served as Chairman of the University of Miami Miller School of Medicine Department of Urology and is currently a Professor at the Miller School of Medicine. Born in Cleveland, Soloway received his B.S. from Northwestern University in Chicago, Il (1961–1964) and completed his M.D. and residency at Case Western Reserve University School of Medicine in Cleveland, Ohio (1964–1970). He completed a fellowship at the National Cancer Institute of the National Institute of Health in Bethesda, MD (1970–1972). Soloway has received numerous awards for his work as a researcher and teacher, including the American Urological Association's Gold Cystoscope Award “For the individual who has contributed most to the field of urology within ten years of completion of his residency program” (1984), Mosby Scholarship for Scholastic Excellence (1967), North Central Section of American Urological Association Traveling Fellowship Award (1972) and many others.

An artificial urinary sphincter (AUS) is an implanted device to treat moderate to severe stress urinary incontinence, most commonly in men. The AUS is designed to supplement the function of the natural urinary sphincter that restricts urine flow out of the bladder.

If medical treatment is not effective, surgery may need to be performed for benign prostatic hyperplasia.

Terence John MillinFRCSI FRCS LRCP was a British-born Irish urological surgeon, who in 1945, introduced a surgical treatment of benign large prostates using the retropubic prostatectomy, later known as the Millin's prostatectomy, where he approached the prostate from behind the pubic bone and through the prostatic capsule, removing the prostate through the retropubic space and hence avoided cutting into the bladder. It superseded the technique of transvesical prostatectomy used by Peter Freyer, where the prostate was removed through the bladder.