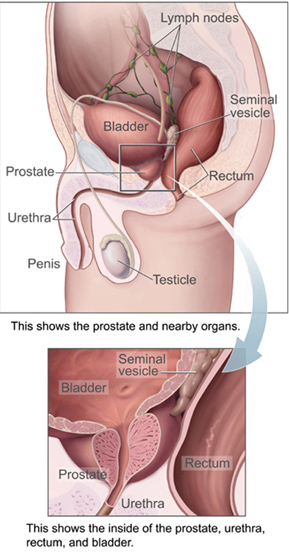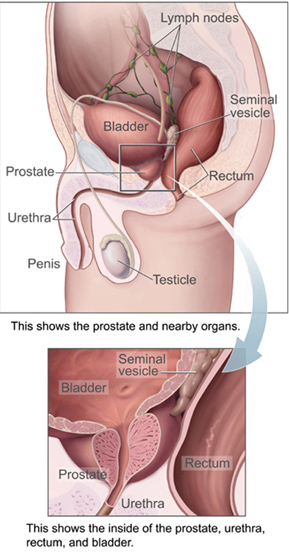
The prostate is an accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found in all male mammals. It differs between species anatomically, chemically, and physiologically. Anatomically, the prostate is found below the bladder, with the urethra passing through it. It is described in gross anatomy as consisting of lobes and in microanatomy by zone. It is surrounded by an elastic, fibromuscular capsule and contains glandular tissue, as well as connective tissue.
Articles related to anatomy include:

The seminal vesicles are a pair of convoluted tubular accessory glands that lie behind the urinary bladder of male mammals. They secrete fluid that largely composes the semen.
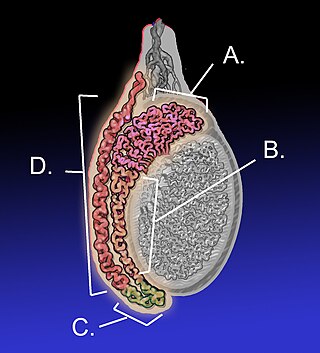
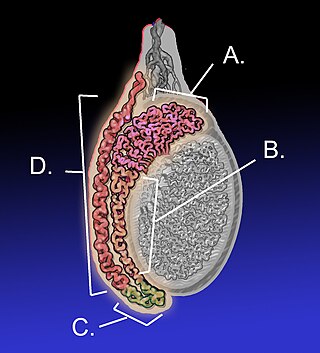
The epididymis is an elongated tubular genital organ attached to the posterior side of each one of the two male reproductive glands, the testicles. It is a single, narrow, tightly coiled tube in adult humans, 6 to 7 centimetres in length; uncoiled the tube would be approximately 6 m long. It connects the testicle to the vas deferens in the male reproductive system. The epididymis serves as an interconnection between the multiple efferent ducts at the rear of a testicle (proximally), and the vas deferens (distally). Its primary function is the storage, maturation and transport of sperm cells.

The ejaculatory ducts are paired structures in the male reproductive system. Each ejaculatory duct is formed by the union of the vas deferens with the duct of the seminal vesicle. They pass through the prostate, and open into the urethra above the seminal colliculus. During ejaculation, semen passes through the prostate gland, enters the urethra and exits the body via the urinary meatus.

The spermatic cord is the cord-like structure in males formed by the vas deferens and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an extension of the peritoneum that passes through the transversalis fascia. Each testicle develops in the lower thoracic and upper lumbar region and migrates into the scrotum. During its descent it carries along with it the vas deferens, its vessels, nerves etc. There is one on each side.

The mesonephric duct, also known as the Wolffian duct, archinephric duct, Leydig's duct or nephric duct, is a paired organ that develops in the early stages of embryonic development in humans and other mammals. It is an important structure that plays a critical role in the formation of male reproductive organs. The duct is named after Caspar Friedrich Wolff, a German physiologist and embryologist who first described it in 1759.

The cremaster muscle is a paired structure made of thin layers of striated and smooth muscle that covers the testicles and the spermatic cords in human males. It consists of the lateral and medial parts. Cremaster is an involuntary muscle, responsible for the cremasteric reflex; a protective and physiologic superficial reflex of the testicles. The reflex raises and lowers the testicles in order to keep them protected. Along with the dartos muscle of the scrotum, it regulates testicular temperature, thus aiding the process of spermatogenesis.

The inguinal canal is a passage in the anterior abdominal wall on each side of the body, which in males, convey the spermatic cords and in females, the round ligament of the uterus. The inguinal canals are larger and more prominent in males.

The male reproductive system consists of a number of sex organs that play a role in the process of human reproduction. These organs are located on the outside of the body, and within the pelvis.

The human reproductive system includes the male reproductive system, which functions to produce and deposit sperm, and the female reproductive system, which functions to produce egg cells and to protect and nourish the fetus until birth. Humans have a high level of sexual differentiation. In addition to differences in nearly every reproductive organ, there are numerous differences in typical secondary sex characteristics.
Hypospermia is a condition in which a man has an unusually low ejaculate volume, less than 1.5 mL. It is the opposite of hyperspermia, which is a semen volume of more than 5.5 mL. It should not be confused with oligospermia, which means low sperm count. Normal ejaculate when a man is not drained from prior sex and is suitably aroused is around 1.5–6 mL, although this varies greatly with mood, physical condition, and sexual activity. Of this, around 1% by volume is sperm cells. The U.S.-based National Institutes of Health defines hypospermia as a semen volume lower than 2 mL on at least two semen analyses.

The testicular artery is a branch of the abdominal aorta that supplies blood to the testicle. It is a paired artery, with one for each of the testicles.

The testicular vein, the male gonadal vein, carries deoxygenated blood from its corresponding testis to the inferior vena cava or one of its tributaries. It is the male equivalent of the ovarian vein, and is the venous counterpart of the testicular artery.

The artery to the ductus deferens is an artery in males that provides blood to the ductus deferens.

The vesical nervous plexus arises from the forepart of the pelvic plexus. The nerves composing it are numerous, and contain a large proportion of spinal nerve fibers. They accompany the vesicle arteries, and are distributed to the sides and fundus of the bladder. Numerous filaments also pass to the seminal vesicles and vas deferens; those accompanying the vas deferens join, on the spermatic cord, with branches from the spermatic plexus.
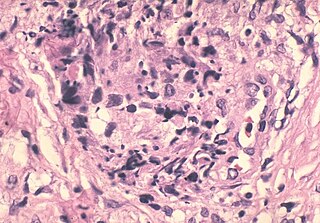
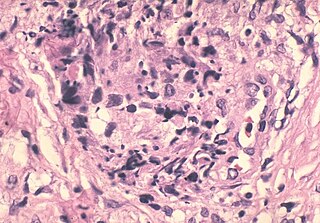
A sperm granuloma is a lump of leaked sperm that appears along the vasa deferentia or epididymides in vasectomized individuals. While the majority of sperm granulomas are present along the vas deferens, the rest of them form at the epididymis. Sperm granulomas range in size, from one millimeter to one centimeter. They consist of a central mass of degenerating sperm surrounded by tissue containing blood vessels and immune system cells. Sperm granulomas may also have a yellow, white, or cream colored center when cut open. While some sperm granulomas can be painful, most of them are painless and asymptomatic. Sperm granulomas can appear as a result of surgery, trauma, or an infection. They can appear as early as four days after surgery and fully formed ones can appear as late as 208 days later.

In most terrestrial mammals, the scrotum or scrotal sac is a part of the external male genitalia located at the base of the penis. It consists of a sac of skin containing the external spermatic fascia, testicles, epididymides, and vasa deferentia. The scrotum will usually tighten when exposed to cold temperatures.

The reproductive system of gastropods varies greatly from one group to another within this very large and diverse taxonomic class of animals. Their reproductive strategies also vary greatly.
The epididymis, which is a tube that connects a testicle to a vas deferens in the male reproductive system, evolved by retention of the mesonephric duct during regression and replacement of the mesonephros with the metanephric kidney. Similarly, during embryological involution of the paired mesonephric kidneys, each mesonephric duct is retained to become the epididymis, vas deferens, seminal vesicle and ejaculatory duct. In reptiles and birds both the testes and excurrent ducts occur in an intra-abdominal location (testicond). Primitive mammals, such as the monotremes (prototheria), also are testicond. Marsupial (metatheria) and placental (eutheria) mammals exhibit differing degrees of testicular descent into an extra-abdominal scrotum. In scrotal mammals the epididymis is attached to the testes in an extra-abdominal position where the cauda epididymis extends beyond the lowest extremity of the testis. Hence, the cauda epididymis is exposed to the coolest of temperatures compared to all other reproductive structures.