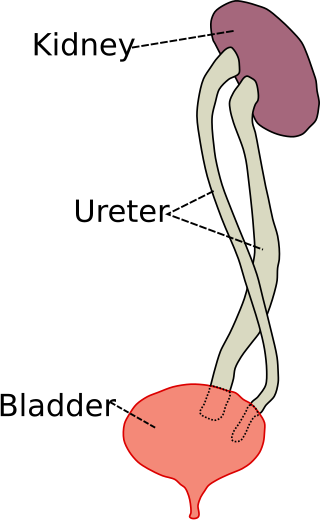
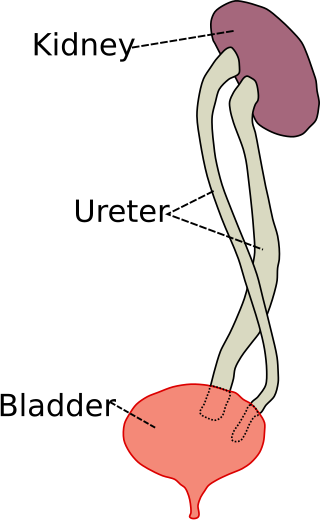
The bladder is a hollow organ in humans and other vertebrates that stores urine from the kidneys. In placental mammals, urine enters the bladder via the ureters and exits via the urethra during urination. In humans, the bladder is a distensible organ that sits on the pelvic floor. The typical adult human bladder will hold between 300 and 500 ml before the urge to empty occurs, but can hold considerably more.

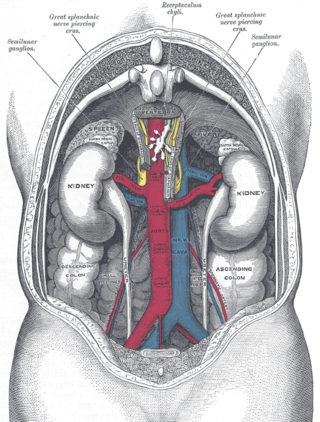
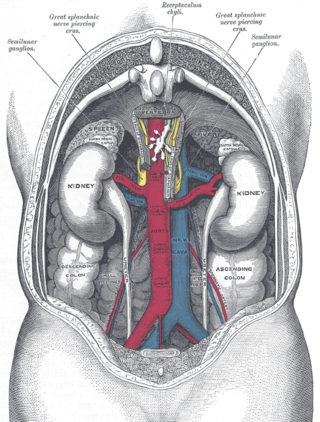
The human urinary system, also known as the urinary tract or renal system, consists of the kidneys, ureters, bladder, and the urethra. The purpose of the urinary system is to eliminate waste from the body, regulate blood volume and blood pressure, control levels of electrolytes and metabolites, and regulate blood pH. The urinary tract is the body's drainage system for the eventual removal of urine. The kidneys have an extensive blood supply via the renal arteries which leave the kidneys via the renal vein. Each kidney consists of functional units called nephrons. Following filtration of blood and further processing, wastes exit the kidney via the ureters, tubes made of smooth muscle fibres that propel urine towards the urinary bladder, where it is stored and subsequently expelled through the urethra during urination. The female and male urinary system are very similar, differing only in the length of the urethra.
The excretory system is a passive biological system that removes excess, unnecessary materials from the body fluids of an organism, so as to help maintain internal chemical homeostasis and prevent damage to the body. The dual function of excretory systems is the elimination of the waste products of metabolism and to drain the body of used up and broken down components in a liquid and gaseous state. In humans and other amniotes, most of these substances leave the body as urine and to some degree exhalation, mammals also expel them through sweating.

The seminal vesicles are a pair of convoluted tubular accessory glands that lie behind the urinary bladder of male mammals. They secrete fluid that largely composes the semen.

Hydronephrosis describes hydrostatic dilation of the renal pelvis and calyces as a result of obstruction to urine flow downstream. Alternatively, hydroureter describes the dilation of the ureter, and hydronephroureter describes the dilation of the entire upper urinary tract.
Horseshoe kidney, also known as ren arcuatus, renal fusion or super kidney, is a congenital disorder affecting about 1 in 500 people that is more common in men, often asymptomatic, and usually diagnosed incidentally. In this disorder, the patient's kidneys fuse to form a horseshoe-shape during development in the womb. The fused part is the isthmus of the horseshoe kidney. The abnormal anatomy can affect kidney drainage resulting in increased frequency of kidney stones and urinary tract infections as well as increase risk of certain renal cancers.
Renal colic, also known as ureteric colic, is a type of abdominal pain commonly caused by obstruction of ureter from dislodged kidney stones. The most frequent site of obstruction is the vesico-ureteric junction (VUJ), the narrowest point of the upper urinary tract. Acute obstruction and the resultant urinary stasis can distend the ureter (hydroureter) and cause a reflexive peristaltic smooth muscle spasm, which leads to a very intense visceral pain transmitted via the ureteric plexus.
Ureteroscopy is an examination of the upper urinary tract, usually performed with a ureteroscope that is passed through the urethra and the bladder, and then directly into the ureter. The procedure is useful in the diagnosis and treatment of disorders such as kidney stones and urothelial carcinoma of the upper urinary tract. Smaller stones in the bladder or lower ureter can be removed in one piece, while bigger ones are usually broken before removal during ureteroscopy.

Vesicoureteral reflux (VUR), also known as vesicoureteric reflux, is a condition in which urine flows retrograde, or backward, from the bladder into one or both ureters and then to the renal calyx or kidneys. Urine normally travels in one direction from the kidneys to the bladder via the ureters, with a one-way valve at the vesicoureteral (ureteral-bladder) junction preventing backflow. The valve is formed by oblique tunneling of the distal ureter through the wall of the bladder, creating a short length of ureter (1–2 cm) that can be compressed as the bladder fills. Reflux occurs if the ureter enters the bladder without sufficient tunneling, i.e., too "end-on".
In urology, voiding cystourethrography (VCUG) is a frequently performed technique for visualizing a person's urethra and urinary bladder while the person urinates (voids). It is used in the diagnosis of vesicoureteral reflux, among other disorders. The technique consists of catheterizing the person in order to fill the bladder with a radiocontrast agent, typically diatrizoic acid. Under fluoroscopy the radiologist watches the contrast enter the bladder and looks at the anatomy of the patient. If the contrast moves into the ureters and back into the kidneys, the radiologist makes the diagnosis of vesicoureteral reflux, and gives the degree of severity a score. The exam ends when the person voids while the radiologist is watching under fluoroscopy. Consumption of fluid promotes excretion of contrast media after the procedure. It is important to watch the contrast during voiding, because this is when the bladder has the most pressure, and it is most likely this is when reflux will occur. Despite this detailed description of the procedure, at least as of 2016 the technique had not been standardized across practices.

A ureteral stent, or ureteric stent, is a thin tube inserted into the ureter to prevent or treat obstruction of the urine flow from the kidney. The length of the stents used in adult patients varies between 24 and 30 cm. Additionally, stents come in differing diameters or gauges, to fit different size ureters. The stent is usually inserted with the aid of a cystoscope. One or both ends of the stent may be coiled to prevent it from moving out of place; this is called a JJ stent, double J stent or pig-tail stent.
Pyelogram is a form of imaging of the renal pelvis and ureter.

A ureterostomy is the creation of a stoma for a ureter or kidney.

Ectopic ureter is a medical condition where the ureter, rather than terminating at the urinary bladder, terminates at a different site. In males this site is usually the urethra, in females this is usually the urethra or vagina. It can be associated with renal dysplasia, frequent urinary tract infections, and urinary incontinence. Ectopic ureters are found in 1 of every 2000–4000 patients, and can be difficult to diagnose, but are most often seen on CT scans.
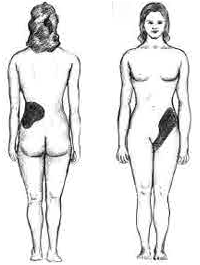
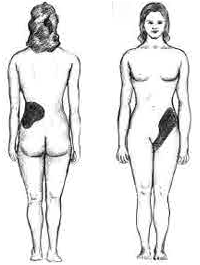
Ovarian vein syndrome is a rare condition in which dilation of the ovarian vein compresses the ureter. This causes chronic or colicky abdominal pain, back pain and/or pelvic pain. The pain can worsen on lying down or between ovulation and menstruation. There can also be an increased tendency towards urinary tract infection or pyelonephritis. The right ovarian vein is most commonly involved, although the disease can be left-sided or affect both sides. It is currently classified as a form of pelvic congestion syndrome.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
Duplicated ureter or duplex collecting system is a congenital condition in which the ureteric bud, the embryological origin of the ureter, splits, resulting in two ureters draining a single kidney. It is the most common renal abnormality, occurring in approximately 1% of the population.

Ureteral cancer is cancer of the ureters, muscular tubes that propel urine from the kidneys to the urinary bladder. It is also known as ureter cancer, renal pelvic cancer, and rarely ureteric cancer or uretal cancer. Cancer in this location is rare. Ureteral cancer becomes more likely in older adults, usually ages 70–80, who have previously been diagnosed with bladder cancer.

Renal ultrasonography is the examination of one or both kidneys using medical ultrasound.
Ureteric stricture (ureteral stricture) is the pathological narrowing of the ureter which may lead to serious complications such as kidney failure.