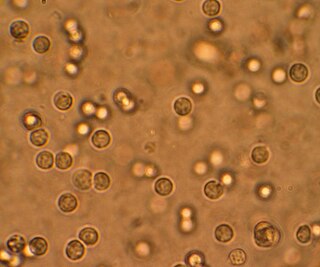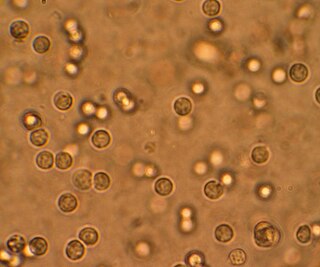
A urinary tract infection (UTI) is an infection that affects a part of the urinary tract. Lower urinary tract infections may involve the bladder (cystitis) or urethra (urethritis) while upper urinary tract infections affect the kidney (pyelonephritis). Symptoms from a lower urinary tract infection include suprapubic pain, painful urination (dysuria), frequency and urgency of urination despite having an empty bladder. Symptoms of a kidney infection, on the other hand, are more systemic and include fever or flank pain usually in addition to the symptoms of a lower UTI. Rarely, the urine may appear bloody. Symptoms may be vague or non-specific at the extremities of age.

Prune belly syndrome is a rare, genetic birth defect affecting about 1 in 40,000 births. About 97% of those affected are male. Prune belly syndrome is a congenital disorder of the urinary system, characterized by a triad of symptoms. The syndrome is named for the mass of wrinkled skin that is often present on the abdomen of those with the disorder.
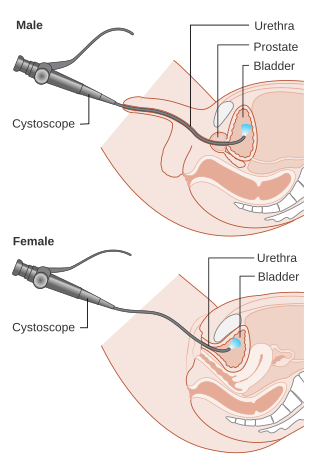
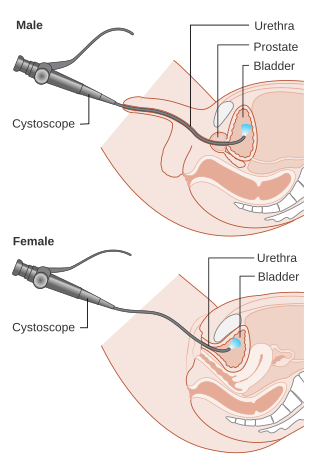
Cystoscopy is endoscopy of the urinary bladder via the urethra. It is carried out with a cystoscope.

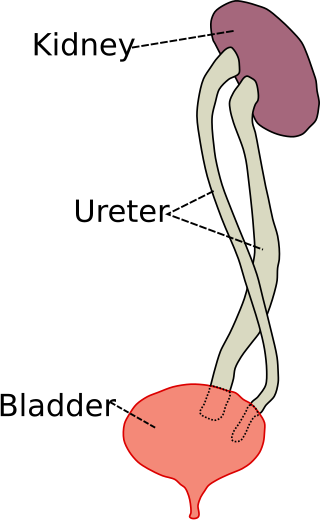
The ureters are tubes composed of smooth muscle that transport urine from the kidneys to the urinary bladder. In an adult human, the ureters typically measure 20 to 30 centimeters in length and about 3 to 4 millimeters in diameter. They are lined with urothelial cells, a form of transitional epithelium, and feature an extra layer of smooth muscle in the lower third to aid in peristalsis. The ureters can be affected by a number of diseases, including urinary tract infections and kidney stone. Stenosis is when a ureter is narrowed, due to for example chronic inflammation. Congenital abnormalities that affect the ureters can include the development of two ureters on the same side or abnormally placed ureters. Additionally, reflux of urine from the bladder back up the ureters is a condition commonly seen in children.

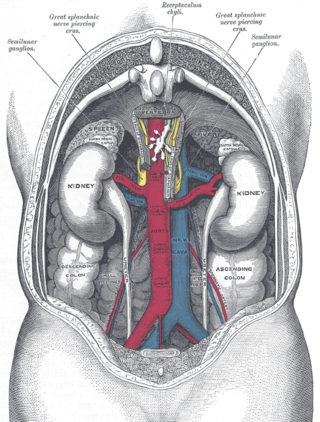
Pyelonephritis is inflammation of the kidney, typically due to a bacterial infection. Symptoms most often include fever and flank tenderness. Other symptoms may include nausea, burning with urination, and frequent urination. Complications may include pus around the kidney, sepsis, or kidney failure.

Hydronephrosis describes hydrostatic dilation of the renal pelvis and calyces as a result of obstruction to urine flow downstream. Alternatively, hydroureter describes the dilation of the ureter, and hydronephroureter describes the dilation of the entire upper urinary tract.

An ileal conduit urinary diversion is one of various surgical techniques for urinary diversion. It has sometimes been referred to as the Bricker ileal conduit after its inventor, Eugene M. Bricker. It is a form of incontinent urostomy, and was developed during the 1940s and is still one of the most used techniques for the diversion of urine after a patient has had their bladder removed, due to its low complication rate and high patient satisfaction level. It is usually used in conjunction with radical cystectomy in order to control invasive bladder cancer.

Posterior urethral valve (PUV) disorder is an obstructive developmental anomaly in the urethra and genitourinary system of male newborns. A posterior urethral valve is an obstructing membrane in the posterior male urethra as a result of abnormal in utero development. It is the most common cause of bladder outlet obstruction in male newborns. The disorder varies in degree, with mild cases presenting late due to milder symptoms. More severe cases can have renal and respiratory failure from lung underdevelopment as result of low amniotic fluid volumes, requiring intensive care and close monitoring. It occurs in about one in 8,000 babies.
In urology, voiding cystourethrography (VCUG) is a frequently performed technique for visualizing a person's urethra and urinary bladder while the person urinates (voids). It is used in the diagnosis of vesicoureteral reflux, among other disorders. The technique consists of catheterizing the person in order to fill the bladder with a radiocontrast agent, typically diatrizoic acid. Under fluoroscopy the radiologist watches the contrast enter the bladder and looks at the anatomy of the patient. If the contrast moves into the ureters and back into the kidneys, the radiologist makes the diagnosis of vesicoureteral reflux, and gives the degree of severity a score. The exam ends when the person voids while the radiologist is watching under fluoroscopy. Consumption of fluid promotes excretion of contrast media after the procedure. It is important to watch the contrast during voiding, because this is when the bladder has the most pressure, and it is most likely this is when reflux will occur. Despite this detailed description of the procedure, at least as of 2016 the technique had not been standardized across practices.

A ureteral stent, or ureteric stent, is a thin tube inserted into the ureter to prevent or treat obstruction of the urine flow from the kidney. The length of the stents used in adult patients varies between 24 and 30 cm. Additionally, stents come in differing diameters or gauges, to fit different size ureters. The stent is usually inserted with the aid of a cystoscope. One or both ends of the stent may be coiled to prevent it from moving out of place; this is called a JJ stent, double J stent or pig-tail stent.
Pyelogram is a form of imaging of the renal pelvis and ureter.
Reflux nephropathy is kidney damage (nephropathy) due to urine flowing backward (reflux) from the bladder toward the kidneys; the latter is called vesicoureteral reflux (VUR). Longstanding VUR can result in small and scarred kidneys during the first five years of life in affected children. The end results of reflux nephropathy can include high blood pressure, excessive protein loss in the urine, and eventually kidney failure.
Ovarian vein syndrome is a rare condition in which dilation of the ovarian vein compresses the ureter. This causes chronic or colicky abdominal pain, back pain and/or pelvic pain. The pain can worsen on lying down or between ovulation and menstruation. There can also be an increased tendency towards urinary tract infection or pyelonephritis. The right ovarian vein is most commonly involved, although the disease can be left-sided or affect both sides. It is currently classified as a form of pelvic congestion syndrome.
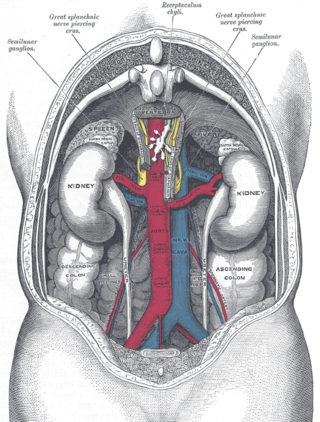
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
Bladder outlet obstruction occurs when urine is unable to flow from the kidneys through the ureters and out of the bladder through the urethra. Decreased flow of urine leads to swelling of the urinary tract, called hydronephrosis. This process of decreased flow of urine through the urinary tract can begin as early as during intrauterine life and it prevents normal development of fetal kidneys and fetal urine. Low levels of fetal urine leads to low amniotic fluid levels and incomplete lung maturation. Older children and adults can also experience bladder outlet obstruction; however, this process is usually reversible and isn't associated with as many poor outcomes as in infants with congenital bladder outlet obstruction.
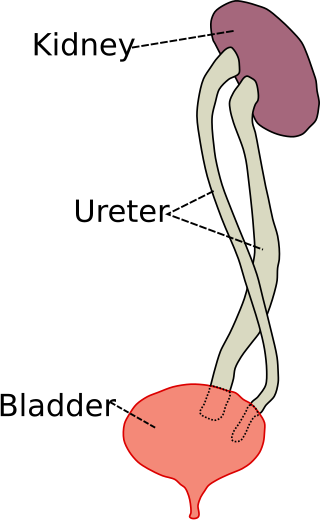
Duplicated ureter or duplex collecting system is a congenital condition in which the ureteric bud, the embryological origin of the ureter, splits, resulting in two ureters draining a single kidney. It is the most common renal abnormality, occurring in approximately 1% of the population.

Fraley syndrome is a condition where the superior infundibulum of the upper calyx of the kidney is obstructed by the crossing renal artery branch, causing distension and dilatation of the calyx and presenting clinically as haematuria and nephralgia. Furthermore, when the renal artery obstructs the proximal collecting system, filling defects can occur anywhere in the calyces, pelvis, or ureter.

Ureteral cancer is cancer of the ureters, muscular tubes that propel urine from the kidneys to the urinary bladder. It is also known as ureter cancer, renal pelvic cancer, and rarely ureteric cancer or uretal cancer. Cancer in this location is rare. Ureteral cancer becomes more likely in older adults, usually ages 70–80, who have previously been diagnosed with bladder cancer.

Renal ultrasonography is the examination of one or both kidneys using medical ultrasound.
Ureteric stricture (ureteral stricture) is the pathological narrowing of the ureter which may lead to serious complications such as kidney failure.