Related Research Articles

Cystic fibrosis (CF) is a genetic disorder that affects mostly the lungs, but also the pancreas, liver, kidneys, and intestine. Long-term issues include difficulty breathing and coughing up mucus as a result of frequent lung infections. Other signs and symptoms may include sinus infections, poor growth, fatty stool, clubbing of the fingers and toes, and infertility in most males. Different people may have different degrees of symptoms.
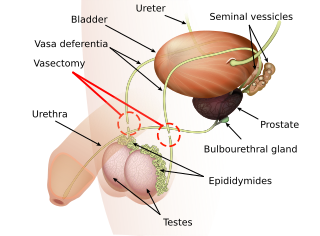
Vasectomy is an elective surgical procedure for male sterilization or permanent contraception. During the procedure, the male vasa deferentia are cut and tied or sealed so as to prevent sperm from entering into the urethra and thereby prevent fertilization of a female through sexual intercourse. Vasectomies are usually performed in a physician's office, medical clinic, or, when performed on an animal, in a veterinary clinic. Hospitalization is not normally required as the procedure is not complicated, the incisions are small, and the necessary equipment routine.

The seminal vesicles are a pair of two convoluted tubular glands that lie behind the urinary bladder of some male mammals. They secrete fluid that partly composes the semen.

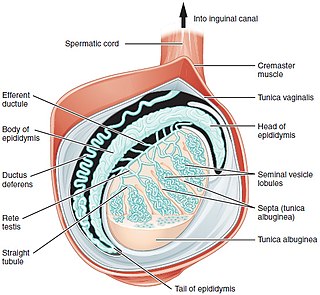
The epididymis is a tube that connects a testicle to a vas deferens in the male reproductive system. It is present in all male reptiles, birds, and mammals. It is a single, narrow, tightly-coiled tube in adult humans, 6 to 7 meters in length connecting the efferent ducts from the rear of each testicle to its vas deferens.

The vas deferens, or ductus deferens, is part of the male reproductive system of many vertebrates. The ducts transport sperm from the epididymis to the ejaculatory ducts in anticipation of ejaculation. The vas deferens is a partially coiled tube which exits the abdominal cavity through the inguinal canal.
Renal agenesis is a medical condition in which one (unilateral) or both (bilateral) fetal kidneys fail to develop.

Persistent Müllerian duct syndrome (PMDS) is the presence of Müllerian duct derivatives in what would be considered a genetically and otherwise physically normal male animal by typical human based standards. In humans, PMDS typically is due to an autosomal recessive congenital disorder and is considered by some to be a form of pseudohermaphroditism due to the presence of Müllerian derivatives.

Spermatocele is a fluid-filled cyst that develops at the head of the epididymis. The fluid is usually a clear or milky white color and may contain sperm. Spermatoceles are typically filled with spermatozoa and they can vary in size from several millimeters to many centimeters. Small spermatoceles are relatively common, occurring in an estimated 30 percent of males. They are generally not painful. However, some people may experience discomfort such as a dull pain in the scrotum from larger spermatoceles. They are not cancerous, nor do they cause an increased risk of testicular cancer. Additionally, unlike varicoceles, they do not reduce fertility.

Cystic fibrosis transmembrane conductance regulator (CFTR) is a membrane protein and chloride channel in vertebrates that is encoded by the CFTR gene.

Vas-occlusive contraception is a form of male contraception that blocks sperm transport in the vas deferens, the tubes that carry sperm from the epididymis to the ejaculatory ducts.
Vasovasostomy is a surgery by which vasectomies are partially reversed. Another surgery for vasectomy reversal is vasoepididymostomy.

The human reproductive system includes the male reproductive system which functions to produce and deposit sperm; and the female reproductive system which functions to produce egg cells, and to protect and nourish the fetus until birth. Humans have a high level of sexual differentiation. In addition to differences in nearly every reproductive organ, there are numerous differences in typical secondary sex characteristics.

Azoospermia is the medical condition of a man whose semen contains no sperm. It is associated with male infertility, but many forms are amenable to medical treatment. In humans, azoospermia affects about 1% of the male population and may be seen in up to 20% of male infertility situations in Canada.
Terms oligospermia, oligozoospermia, and low sperm count refer to semen with a low concentration of sperm and is a common finding in male infertility. Often semen with a decreased sperm concentration may also show significant abnormalities in sperm morphology and motility. There has been interest in replacing the descriptive terms used in semen analysis with more quantitative information.
Hypospermia is a condition in which humans have an unusually low ejaculate volume, less than 1.5 mL. It is the opposite of hyperspermia, which is a semen volume of more than 5.5 mL. It should not be confused with oligospermia, which means low sperm count. Normal ejaculate when a man is not drained from prior sex and is suitably aroused is around 1.5–6 mL, although this varies greatly with mood, physical condition, and sexual activity. Of this, around 1% by volume is sperm cells. The U.S.-based National Institutes of Health defines hypospermia as a semen volume lower than 2 mL on at least two semen analyses.
Male infertility refers to a sexually mature male's inability to impregnate a fertile female. In humans it accounts for 40–50% of infertility. It affects approximately 7% of all men. Male infertility is commonly due to deficiencies in the semen, and semen quality is used as a surrogate measure of male fecundity. More recently, advance sperm analyses that examine intracellular sperm components are being developed.
Testicular sperm extraction (TESE) is a surgical procedure in which a small portion of tissue is removed from the testicle and any viable sperm cells from that tissue are extracted for use in further procedures, most commonly intracytoplasmic sperm injection (ICSI) as part of in vitro fertilisation (IVF). TESE is often recommended to patients who cannot produce sperm by ejaculation due to azoospermia.
Post-vasectomy pain syndrome (PVPS) is a chronic and sometimes debilitating genital pain condition that may develop immediately or several years after vasectomy. Because this condition is a syndrome, there is no single treatment method, therefore efforts focus on mitigating/relieving the individual patient's specific pain. When pain in the epididymides is the primary symptom, post-vasectomy pain syndrome is often described as congestive epididymitis.
Vasectomy reversal is a term used for surgical procedures that reconnect the male reproductive tract after interruption by a vasectomy. Two procedures are possible at the time of vasectomy reversal: vasovasostomy and vasoepididymostomy. Although vasectomy is considered a permanent form of contraception, advances in microsurgery have improved the success of vasectomy reversal procedures. The procedures remain technically demanding and expensive, and may not restore the pre-vasectomy condition.
Vasoepididymostomy or epididymovasostomy is a surgery by which vasectomies are reversed. It involves connection of the severed vas deferens to the epididymis and is more technically demanding than the vasovasostomy.
References
- ↑ Donohue, R. E.; Fauver, H. E. (1989-02-24). "Unilateral absence of the vas deferens. A useful clinical sign". JAMA. 261 (8): 1180–1182. doi:10.1001/jama.1989.03420080100041. PMID 2604761.
- ↑ Chawla, S (October 1999). "Congenital Unilateral Absence of the Vas Deferens". Medical Journal Armed Forces India. 55 (4): 375. doi:10.1016/S0377-1237(17)30530-0. PMC 5531955 . PMID 28790624.
- ↑ Miller, Sarah; Couture, Sophie; James, Gareth; Plourde, Simon; Rioux, Jacky; Labrecque, Michel (October 2016). "Unilateral absence of vas deferens: prevalence among 23,013 men seeking vasectomy". International Braz J Urol. 42 (5): 1010–1017. doi:10.1590/S1677-5538.IBJU.2015.0717. PMC 5066900 . PMID 27509370.
- ↑ Online Mendelian Inheritance in Man (OMIM): VAS DEFERENS, CONGENITAL BILATERAL APLASIA OF; CBAVD - 277180
- ↑ Grangeia A, Sá R, Carvalho F, et al. (2007). "Molecular characterization of the cystic fibrosis transmembrane conductance regulator gene in congenital absence of the vas deferens". Genet. Med. 9 (3): 163–72. doi: 10.1097/GIM.0b013e3180318aaf . PMID 17413420.
- ↑ Chillón M, Casals T, Mercier B, Bassas L, Lissens W, Silber S, Romey MC, Ruiz-Romero J, Verlingue C, Claustres M, et al. (1995). "Mutations in the cystic fibrosis gene in patients with congenital absence of the vas deferens". N. Engl. J. Med. 332 (22): 1475–80. doi:10.1056/NEJM199506013322204. hdl: 2445/44112 . PMID 7739684.
- 1 2 Dörk T, Dworniczak B, Aulehla-Scholz C, Wieczorek D, Böhm I, Mayerova A, Seydewitz HH, Nieschlag E, Meschede D, Horst J, Pander HJ, Sperling H, Ratjen F, Passarge E, Schmidtke J, Stuhrmann M (1997). "Distinct spectrum of CFTR gene mutations in congenital absence of vas deferens". Hum. Genet. 100 (3–4): 365–377. doi:10.1007/s004390050518. PMID 9272157. S2CID 24344109.
- ↑ McCallum T, Milunsky J, Munarriz R, Carson R, Sadeghi-Nejad H, Oates R (2001). "Unilateral renal agenesis associated with congenital bilateral absence of the vas deferens: phenotypic findings and genetic considerations". Hum. Reprod. 16 (2): 282–288. doi: 10.1093/humrep/16.2.282 . PMID 11157821.
- ↑ Rosenstein BJ, Cutting GR (1998). "The diagnosis of cystic fibrosis: a consensus statement. Cystic Fibrosis Foundation Consensus Panel". J. Pediatr. 132 (4): 589–95. doi:10.1016/S0022-3476(98)70344-0. PMID 9580754.
- ↑ Lotti, F.; Maggi, M. (2014). "Ultrasound of the male genital tract in relation to male reproductive health" (PDF). Human Reproduction Update. 21 (1): 56–83. doi: 10.1093/humupd/dmu042 . ISSN 1355-4786. PMID 25038770.